Published online Jun 28, 2021. doi: 10.3748/wjg.v27.i24.3483
Peer-review started: February 1, 2021
First decision: May 1, 2021
Revised: May 6, 2021
Accepted: May 25, 2021
Article in press: May 25, 2021
Published online: June 28, 2021
Pancreatic cancer remains one of medicine’s largest areas of unmet need. With five-year survival rates of < 8%, little improvement has been made in the last 50 years. Typically presenting with advance stage disease, treatment options are limited. To date, surgery remains the only potentially curative option, however, with such late disease presentation, the majority of patients are unresectable. Thus, new therapeutic options and a greater understanding of the complex stromal interactions within the tumour microenvironment are sorely needed to revise the dismal outlook for pancreatic cancer patients. Natural killer (NK) cells are crucial effector units in cancer immunosurveillance. Often used as a prognostic biomarker in a range of malignancies, NK cells have received much attention as an attractive target for immunotherapies, both as cell therapy and as a pharmaceutical target. Despite this interest, the role of NK cells in pancreatic cancer remains poorly defined. Nevertheless, increasing evidence of the importance of NK cells in this dismal prognosis disease is beginning to come to light. Here, we review the role of NK cells in pancreatic cancer, examine the complex interactions of these crucial effector units within pancreatic cancer stroma and shed light on the increasingly attractive use of NK cells as therapy.
Core Tip: Increasing evidence has found natural killer (NK) cells to be crucial players in the prognosis and progression of cancer. Whilst pancreatic cancer remains one of medicine’s largest areas of unmet need, NK cells may prove to be an exciting new therapeutic option for pancreatic cancer patients. Here we provide an overview of the complex interactions between NK cells and pancreatic cancer stroma, suggest a role for NK cells as prognostic biomarkers and highlight exciting new NK cell-based treatment options which may transform the therapeutic landscape of pancreatic cancer.
- Citation: Fincham REA, Delvecchio FR, Goulart MR, Yeong JPS, Kocher HM. Natural killer cells in pancreatic cancer stroma. World J Gastroenterol 2021; 27(24): 3483-3501
- URL: https://www.wjgnet.com/1007-9327/full/v27/i24/3483.htm
- DOI: https://dx.doi.org/10.3748/wjg.v27.i24.3483
Pancreatic cancer is a malignancy with a dismal prognosis. Set to become the second leading cause of cancer-related death worldwide by 2030, little progress has been made in the treatment of pancreatic cancer over the past five decades[1,2]. Surgery remains the only potentially curative option, however, with the majority of patients typically presenting with advance stage disease, most cases are unresectable. Further to this, with approximately 80% of surgery patients relapsing, frequently within two years, pancreatic cancer has solidified itself as one of medicine’s most urgent areas of unmet need[3].
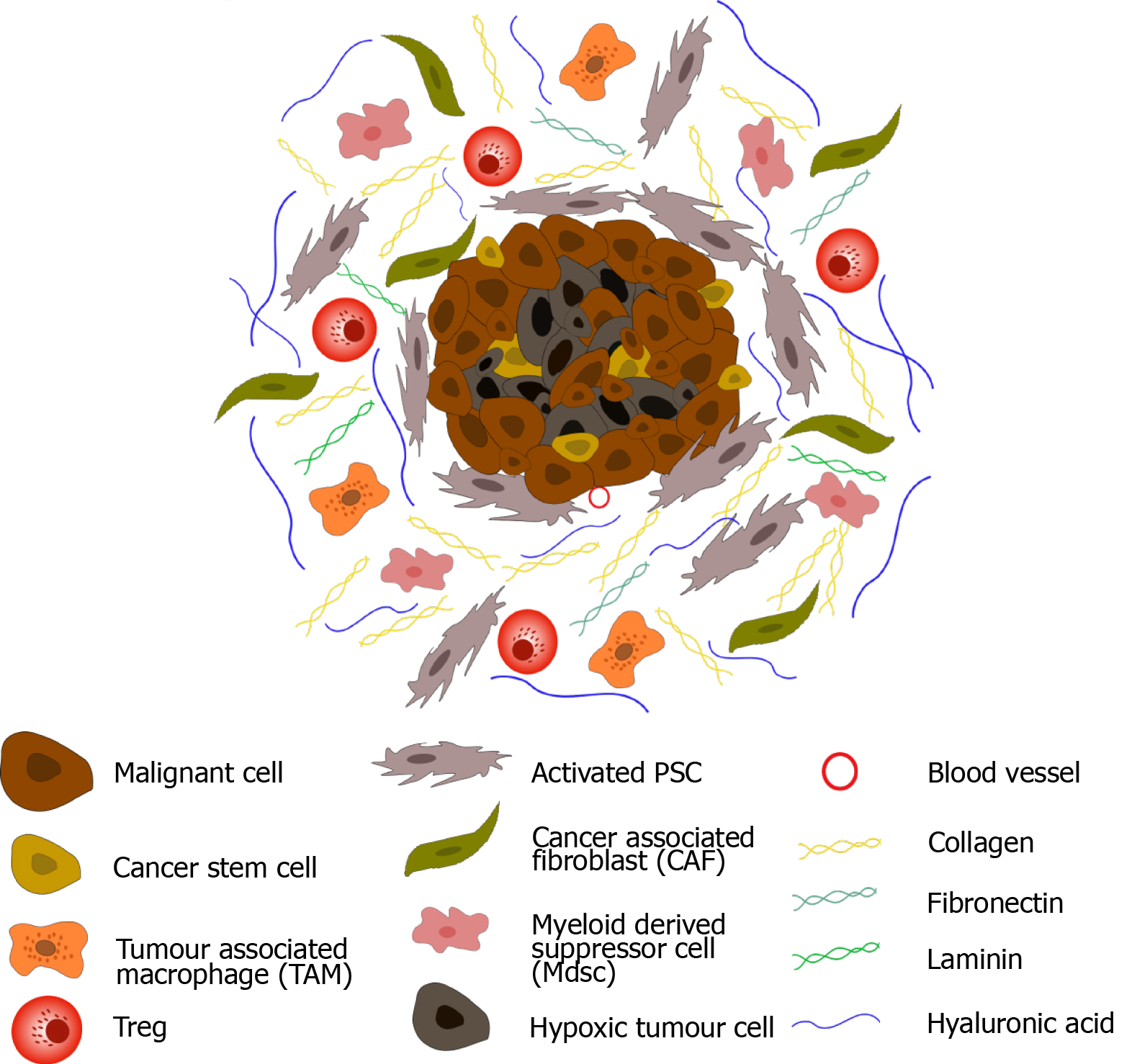
Characterised by its strong desmoplastic reaction, the pancreatic ductal adenocarcinoma (PDAC) tumour microenvironment (TME) plays a crucial role in disease progression[4,5]. Primary tumour sites display extensive fibrosis characterised by overexpression of extracellular matrix proteins (such as laminin, collagen and fibronectin) and activation of fibroblastic cells. Multiple cell types, both cancer and stromal, are present in the pancreatic TME, including; pancreatic stellate cells (PSCs), myeloid-derived suppressor cells (MDSCs), tumour associated macrophages (TAMs) and regulatory T-cells (Tregs), amongst many other cell types[6,7]. The dense fibrosis associated with PDAC (largely orchestrated by PSCs) results in tumour hypoxia, a feature characteristic of PDAC, which is exacerbated by the secretion of anti-angiogenic factors (such as endostatin and angiostatin) by both pancreatic cancer and stellate cells[6,8]. Development of a hypoxic TME has been linked to disease aggressiveness and progression, as well as chemotherapy resistance. Importantly, in addition to developing resistance to chemotherapeutics, the pancreatic TME is highly immunosuppressive, limiting the efficacy of the immune-mediated cancer surveillance[6]. MDSCs release reactive oxygen species (ROS) and reactive nitrogen species which have been shown to inhibit T cell proliferation and migration into the TME. In addition, release of immunosuppressive cytokines including interleukin (IL)-10 and transforming growth factor beta (TGF-β) sustains the development of Tregs which further modulate the TME[9]. Tregs secrete immunosuppressive cytokines such as IL-10 and TGF-β which recruit additional immunosuppressive cells to the TME and stimulate the transition of CD4+ T cells to FoxP3+ regulatory cells, facilitating immune evasion[6,10]. Through the release of IL-10 and TGF-β, tumour associated macrophages are also able to induce T-cell anergy leading to the development of an immune-privileged microenvironment[11]. Finally, pancreatic cancer cells can downregulate Fas, resulting in resistance to CD8+ T cell-induced Fas/FasL apoptosis[6,12]. Key components of the PDAC TME are shown in Figure 1.
NK cells are large granular lymphocytes which are key components of the innate immune system, and are poorly understood compared to other lymphocytes (T and B cells) belonging to the adaptive immune system. Acting as the first line of defence against viral infected and malignant cells[13,14], NK cells are classified as CD56+CD3- cells. This classification can be further sub-divided into two main effector populations: immunomodulatory CD56brightCD16- cells which regulate their function through cytokine release [specifically interferon (IFN)-γ], and cytotoxic CD56dimCD16+ effector cells[14]. Activation of NK cells relies on the balance of signals received from inhibitory and activating cell surface receptors (Figure 2)[13]. Inhibitory receptors, comprised of killer cell immunoglobulin-like receptors (KIRs) and C-type lectin-like receptors, including natural killer group 2 member A (NKG2A), specifically recognisemajor histocompatibility complex (MHC) class 1 molecules. These ligands are highly expressed on non-transformed ‘self’ cells, and consequently prevent harmful activation of NK cells against host cells. Conversely, malignant cells often downregulate the expression of surface MHC-1 molecules to evade detection by T cells. This ‘missing self’ signal prevents the inhibition of the NK cells, resulting in cytotoxic efficacy[13,14]. NK cells can also be negatively regulated by checkpoint proteins such as programme death 1 (PD-1), which binds to its’ ligands programme death ligand 1 and 2 (PDL-1, PDL-2)[13]. Activating receptors include the type 1 transmembrane natural cytotoxicity receptors (NCRs) NKp46 (which is exclusive to NK cells), NKp30 and NKp44 (which are also expressed on T cells), the C-type lectin-like receptors NKG2C and NKG2D, the activating KIRs and the DNAX accessory molecule 1 (DNAM1)[13-15]. Ligands for the activating KIR receptors include the HLA-C2 and HLA-A ligands, however, the interaction between ligand and receptor is less well understood for activating KIRs than for their inhibitory counterparts[16]. NKG2D receptors recognise stress-induced proteins on transformed and virally infected cells. These include the MHC class 1 related genes MICA and MICB and UL-16 binding proteins[16]. Whilst recognising nectin adhesion molecule and the poliovirus receptor, DNAM1 also interacts with the β2 integrin leukocyte function-associated antigen 1 (LFA-1) which is involved in the formation of the immunological synapse[15]. It is important to note that in addition to independent activation, specific combinations of activating receptors are synergistic, increasing the overall signal received by the effector cell and consequently, increasing its cytotoxic response[17].
CD16+ NK cells, in addition to direct receptor-ligand binding, express a propensity to carry out antibody-dependent cellular cytotoxicity (ADCC)[18]. CD16 (FcγRIII) is a transmembrane receptor which can bind the Fc region of IgG1 and IgG3 antibodies, enabling NK cells to kill immunoglobulin labelled cells[16], a crucial concept for monoclonal antibody-based therapies[13].
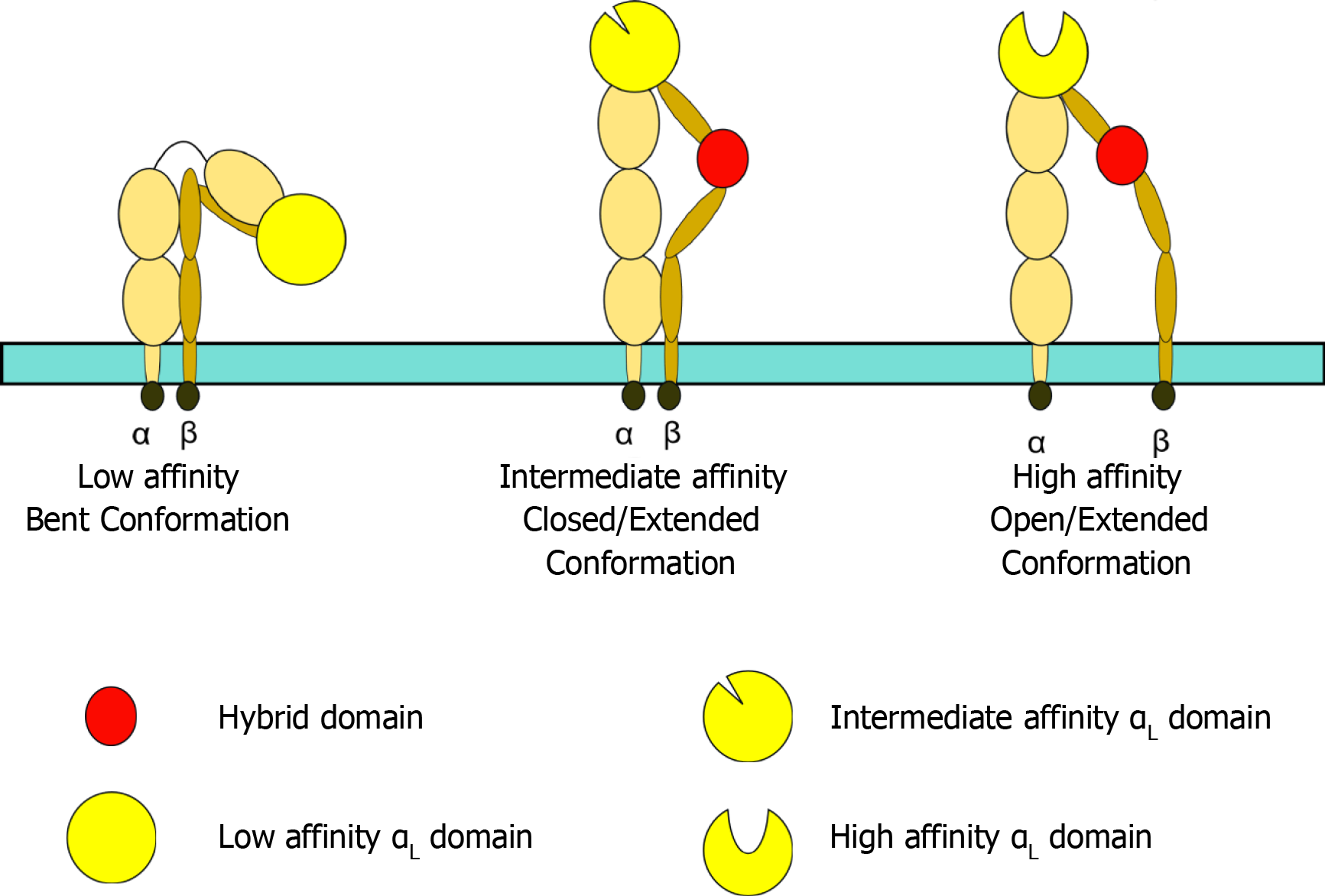
Following initial interactions between activating/inhibitory receptors and target cells, the balance of signals received by the NK cell determines its activation status. If activated, NK cells must form an immunological synapse with the target cell. Formation of this synapse enables stable adhesion, polarisation of cytotoxic granules and subsequent lysis of the target cell. This is achieved through binding of the β2 integrin, LFA-1[17]. Consisting of two chains, αL and β2, LFA-1 is a heterodimer whose reactivity to its ligands (ICAM family members) can be modified via conformational changes. Specifically, a bent conformation exhibits a low affinity for its ligands, intermediate affinity can be achieved through a closed/extended conformation, whilst an open/extended conformation results in high-affinity binding (Figure 3)[17,19,20].
In contrast to T cells, NK cells do not require inside-out signals (such as chemokines and T cell receptor activation) to stimulate LFA-1 binding and can signal auto
Initially identified as a result of their ‘natural’ cytotoxicity towards both syngeneic and allogeneic tumour cells, NK cells have widely demonstrated potent anti-tumoral cytotoxicity[36-38]. However, they are highly heterogeneous both between cancer types and intra-tumourally[36]. Moreover, the variable functional status of NK cells is seen to greatly impact their anti-tumoral efficacy[36]. Upregulation of the inhibitory receptor NKG2A has been associated with NK cell exhaustion and poorer prognosis in patients with liver cancer[39], whilst PD-1 engagement of NK cells has been shown to block the polarisation of lytic granules and impair outside-in integrin signalling[40]. Increased expression of PD-1 on NK cells has also been associated with poorer overall survival in patients with hepatocellular carcinoma[41]. Conversely, high proportions of functionally active NK cells result in favourable outcomes in many cancer types[42]. Retrospective flow cytometric assessment of peripheral blood samples from metastatic prostate cancer patients (Gleason scores between 6-9) followed by univariate Cox regression analysis demonstrated a significant correlation between expression of the activating receptors NKp46 and NKp30, and longer overall survival[42]. Similarly, immunostaining of tissue samples from 98 patients with gastric cancer (stage 1-4) combined with multivariate analysis revealed a positive correlation between NKG2D expression in tumour infiltrating lymphocytes and prolonged OS (hazard ratio 0.34)[43]. With the propensity to exhibit potent anti-tumoral activity, NK cell-based immunotherapy research has flourished in the past few years[36].
NK cell number has been found to convey prognostic significance. Through flow cytometric analysis of PBMCs from resectable PDAC patients (stage Ib-III) both pre- and post-surgery, Hoshikawa et al[44] demonstrated a positive correlation between the percentage of NK cells in peripheral blood and recurrence-free survival, with patients who exhibited high NK levels expressing later disease recurrence. Moreover, univariate and multivariate analysis using the Cox proportional hazard regression model demonstrated NK cell frequency to be the only favourable prognostic factor for recurrence-free survival. Additional factors tested included tumour stage, N status, radicality, age and gender. Importantly, no additional circulating mononuclear cells were included in this analysis. NK cell infiltrate within the TME (assessed by gene expression profile) was also found to be associated with later disease recurrence, however, this was not statistically significant[44]. Assessment of a larger cohort of patients would improve the power of this assessment and may provide further insight into the role of tumour infiltrating NK cells in PDAC.
Finally, gene set enrichment analysis revealed that patients with enriched type I and II IFN signatures within tumour tissues had later disease recurrence. Type I and II IFNs are closely associated with NK cell function. Type I IFNs induce NK cell activation both directly, through binding to type I IFN receptor, or indirectly, through stimulating dendritic cell release of IL-15, whilst type II IFNs (namely IFN-γ) are produced by activated NK cells[45,46]. Moreover, IFNs can induce CXCL10 release, leading to the further recruitment of NK cells to the tumour tissue[44]. Thus, enriched IFN signatures were also concluded to be a positive prognostic biomarker in PDAC[44].
Yang et al[47] also suggest prognostic implication of NK cells in PDAC. High densities of NK cells in peripheral blood samples (analysed by flow cytometry) were found to correlate with poor overall survival in patients with advanced PDAC (stage III/IV) when accompanied by a high neutrophil: lymphocyte ratio (obtained from routine hospital data). NK cell number (HR 1.45), as well as patient age (HR 1.34), neutrophil to lymphocyte ratio (HR 1.48) and absence of metastasis (HR 0.72) were found to be independent prognostic markers following univariate and multivariate Cox regression analysis. It is perhaps prudent to note that subsequent ELISAs to measure release of IFN-γ and TNF-α from NK cells as well as serum IL-2 Levels, a known activator of NK cells, demonstrated lower levels of all three markers in patients with high NK cell densities, although only IFN-γ reached significance. These results suggest a distinct subtype of NK cells with impaired function in PDAC patients and thus prognostic significance may rely not just on NK cell numbers, but on functional subtypes[47]. The results obtained within this study focus solely on peripheral blood circulating NK cells. Further work to classify functional NK cell subtypes within PDAC tumour tissue would provide more conclusive insights into the prognostic significance of these effector cells in PDAC.
NK cells have demonstrated potent anti-tumoral efficacy in murine models of PDAC. Using a transgenic mouse model in which oncogenic transposons for KrasG12V and myristoylated Akt2 were introduced into p53fl/fl mice via intra-pancreatic injection and electroporation, along with plasmids for Cre recombinase and sleeping beauty transposase, Brooks et al[48] demonstrated that neo-adjuvant PD-1 blockade plus adjuvant CD96 inhibition in combination with gemcitabine prevented relapse and facilitated long term remission following resection surgery. To further investigate the role of immune cells in neo-adjuvant and adjuvant treatment of PDAC, mice were injected (intraperitoneal) with anti-CD8 and anti-NK.1.1 depletion antibodies. Pre-operatively, depletion of both CD8+ T cells and NK cells significantly reduced survival when compared to the control. Furthermore, adjuvant NK but not CD8+ depletion was found to impair survival and resulted in an increase in local disease recurrence. In vitro luciferase cytotoxicity assays confirmed NK cell cytolytic efficacy against tumour derived cancer cells, a finding consistent with the results obtained for depletion experiments. Thus, targeting both T and NK cells through immune checkpoint inhibition may confer long term survival benefits in metastatic cases of PDAC[48]. Similarly, in a KrasLSL-G12D p53LSL-R172H Pdx1-Cre (KPC) model of PDAC, NK cell-based adoptive transfer immunotherapy was found to significantly delay tumour growth[49]. In addition, immunostaining of KPC tumours at end time-points revealed significantly elevated areas of necrosis in mice treated with adoptive transfer of NK cells compared to control mice, demonstrating the cytotoxic efficacy of NK cell treatment, a finding replicated through in vitro flow cytometry cytotoxicity assays[49].
Xenograft models of PDAC have also been used to demonstrate the efficacy of ex vivo expansion of NK cells. NOD scid gamma (NSG) mice injected subcutaneously with MiaPaca2 cells demonstrated a significant reduction in tumour growth when treated with adoptive transfer of ex vivo expanded NK cells (versus control group)[50]. This finding demonstrated both successful trafficking of NK cells to the tumour site and tumour control following intravenous injection, suggesting that NK cells may prove an effective systemic treatment in xenograft models of PDAC[50]. It is prudent to note that the nature of this model requires the mice included within the study to be immuno-compromised, and this must be taken into consideration when reviewing the data presented. Employing additional models would add further validity to the therapeutic impact of ex vivo expanded NK cells in murine models of PDAC[50].
Notorious for their resistance to typical anti-proliferative/cytotoxic therapies, cancer stem cells are an important subpopulation involved in cancer progression, metastasis and recurrence. Despite their notoriety, CSCs are preferentially targeted by NK cells in both the autologous and allogeneic setting; an effect which was found to be NKG2D dependent[51]. Metastatic, intra-pancreatic and subcutaneous models of PDAC were established in NSG mice using the PANC-1 cancer cell line. Mice treated with adoptively transferred NK cells were found to have substantial reductions in tumour volume when compared to untreated mice. Flow cytometric analysis also demonstrated a significant reduction in CSC populations in mice treated with adoptive NK cell transfer (denoted by aldehyde and CD24 expression). Moreover, immunostaining revealed co-localisation of NK cells and CSCs within tumour tissues. Ames et al[51] conclude that NK cells possess the ability to identify and preferentially target CSCs in solid tumours. As such, further work investigating the impact of systemic adoptive transfer of NK cells on CSC populations may yield exciting new therapeutic insights into the treatment of this dismal prognosis disease.
Pancreatic tumour cells have developed several methods of NK-cell immune evasion. Murine models of pancreatic cancer specifically designed to express MYC at the Rosa26 Locus, either with or without the Lsl-KrasG12D allele, were used to determine the role of MYC in pancreatic tumour progression. MYC expression was found to drive pancreatic cancer development and accelerate disease progression in precursor lesions initiated by KRAS. Moreover, bulk RNA sequencing of end stage tumours revealed reduced expression of T-cell, B-cell and NK cell markers in tumour tissue, suggesting that immune cell infiltration may be regulated by MYC. GeneGo analysis revealed that allelic activation of both KRAS and MYC resulted in significant downregulation of type I IFN, an effect that was found to be dependent on repressional binding of MYC-interacting zinc finger protein, MIZ1. Deletion of MIZ1 resulted in restoration of NK and B cell infiltration into tumour tissues, an effect ablated upon antibody dependent blockade of type I IFN[52]. Similarly, the oncoprotein Sloan-Kettering Institute has been shown to inhibit SMAD association with the acetyltransferases CBP and p300, which are key regulators of inducible expression of NKG2D ligands on cancer cells, and facilitate repression of gene transcription via histone deacetylases. This results in downregulation of NKG2D ligands on tumoral cells, reducing NKG2D dependent cytotoxicity and facilitating immune evasion[53]. In addition, tumoral cells are seen to exhibit intricate crosstalk with NK effector cells and have been shown to induce functional deregulation[54]. Co-culture with the pancreatic cancer cell line MiaPaca2 was found to induce NK cell anergy via fibrinogen-like protein 2 and was characterised through decreased expression of DNAM-1, IFN-γ and CD107a and increased expression of PD-1[55]. Importantly, when co-cultured, anergic NK cells were seen to induce anergy in naïve NK cells, reducing IFN-γ and CD107a expression[55]. Further work investigating the reversal of NK cell anergy, both tumour-dependent and bystander anergy may lead to novel therapeutic insights, and provide a baseline from which to further challenge PDAC immune evasion.
MHC class-I chain-related molecules A/B (MICA/B) are crucial ligands for the activating receptor NKG2D. Several studies have demonstrated immune evasion as a result of MICA/B shedding by tumour cells. Duan et al[56] demonstrated that high glucose levels, which are widely correlated with pancreatic cancer, could facilitate immune evasion. Specifically, in vitro assays demonstrated a decrease in NK cell induced lysis of pancreatic cancer cell lines (demonstrated by lactate dehydrogenase release assays) when cultured in high glucose conditions. Moreover, western blot and quantitative real-time polymerase chain reaction (PCR) analysis revealed that this decrease in function was a result of reduced expression of MICA/B in cancer cell lines at both the protein and mRNA level. Mechanistically, high glucose was found to inhibit AMP-activated protein kinase signalling, leading to upregulation of the polycomb group protein (PcG) Bmi1, and subsequent promotion of GATA2 expression. This augmentation inhibited expression of MICA/B on pancreatic cancer cells and led to their immune evasion[56]. Similar shedding of the NKG2D ligand has been observed in response to hypoxia. High levels of HIF1α have been correlated with decreased expression of MICA/B on pancreatic tumour cells and also with increased internalisation of the activating receptor NKG2D, suggesting a dual role for the hypoxic TME in NK cell dysfunction[57]. Specifically, immune-histochemical analysis of PDAC patient tumour tissues revealed a significant correlation between MICA surface expression and high HIF1α. Moreover, immune-fluorescent staining of NK cells isolated from patient PBMCs demonstrated clear internalisation of the activating NKG2D receptors as well as MICA/B[57].
Receptor expression is found to be largely augmented in pancreatic cancer patients. Flow cytometric analysis of participant blood samples revealed that expression of the activating receptors DNAM-1 (CD226) and CD96 were significantly reduced in pancreatic cancer patients (stage I-IV) when compared to healthy controls. This downregulation was suggested to lead to NK cell dysfunction and tumour evasion.[58] Downregulation of NKG2D in pancreatic cancer patients has also been correlated to reduced cytotoxicity of the effector cells. In vitro blockade of NKG2D using neutra
Additionally, flow cytometric analysis of cell surface markers following in vitro co-cultures of NK cells derived from healthy PBMCs and pancreatic cancer cell lines revealed downregulation of the NK activating receptors NKG2D, NKp30, NKp46 and DNAM-1. ELISA analysis suggested that this dysfunction was induced as a result of matrix metalloproteinase 9 (MMP9) and Indoleamine 2,3 dioxygenase (IDO) signalling cascades.[60] In addition to downregulation of activating receptors, exposure to MMP9 and IDO also led to decreased TNF-α and IFN-γ production by NK cells, an effect that was reversed upon blockade of MMP9 and IDO using tissue inhibitor of metalloproteinases 1 and 1-Methyl-DL-tryptopan, respectively[60]. This finding was replicated in a comprehensive study of surface receptor expression and cytotoxic granule positive cells in pancreatic (stage II and IV), gastric (stage 0-IV) and colorectal cancer (stage I-IV) patients. Using flow cytometry, Peng et al[61] identified significant downregulation of the activating receptors NKG2D, NKp30, NKp46 and DNAM-1 on NK cells identified in peripheral blood samples from pancreatic cancer patients when compared to healthy controls, whilst expression of the inhibitory receptor KIR3DL1 was significantly upregulated. Moreover, the percentage of perforin positive circulating NK cells was found to be significantly reduced in pancreatic cancer patients. Taken together, these alterations evidence the dysfunction of NK cells observed in malignancy.
Impairment in degranulation was also identified by Jun et al[62]. In an in vitro flow cytometry-based degranulation assay, PBMCs derived from malignant patients, non-malignant patients or healthy controls were mixed with target cells before staining with CD107a. NK cells derived from pancreatic cancer patients showed significantly impaired degranulation when compared to non-malignant and/or healthy control samples. Despite demonstrating impaired cytotoxic capabilities, no significant difference in NK cell IFN-γ production was observed between cancer patients and healthy controls. Importantly, multivariate analysis revealed that tumour-induced NK cell dysfunction correlated with disease stage, suggesting progressive impairment of NK cells with advanced-stage disease. Thus, as previously suggested, NK functional status may prove an attractive prognostic marker in PDAC.
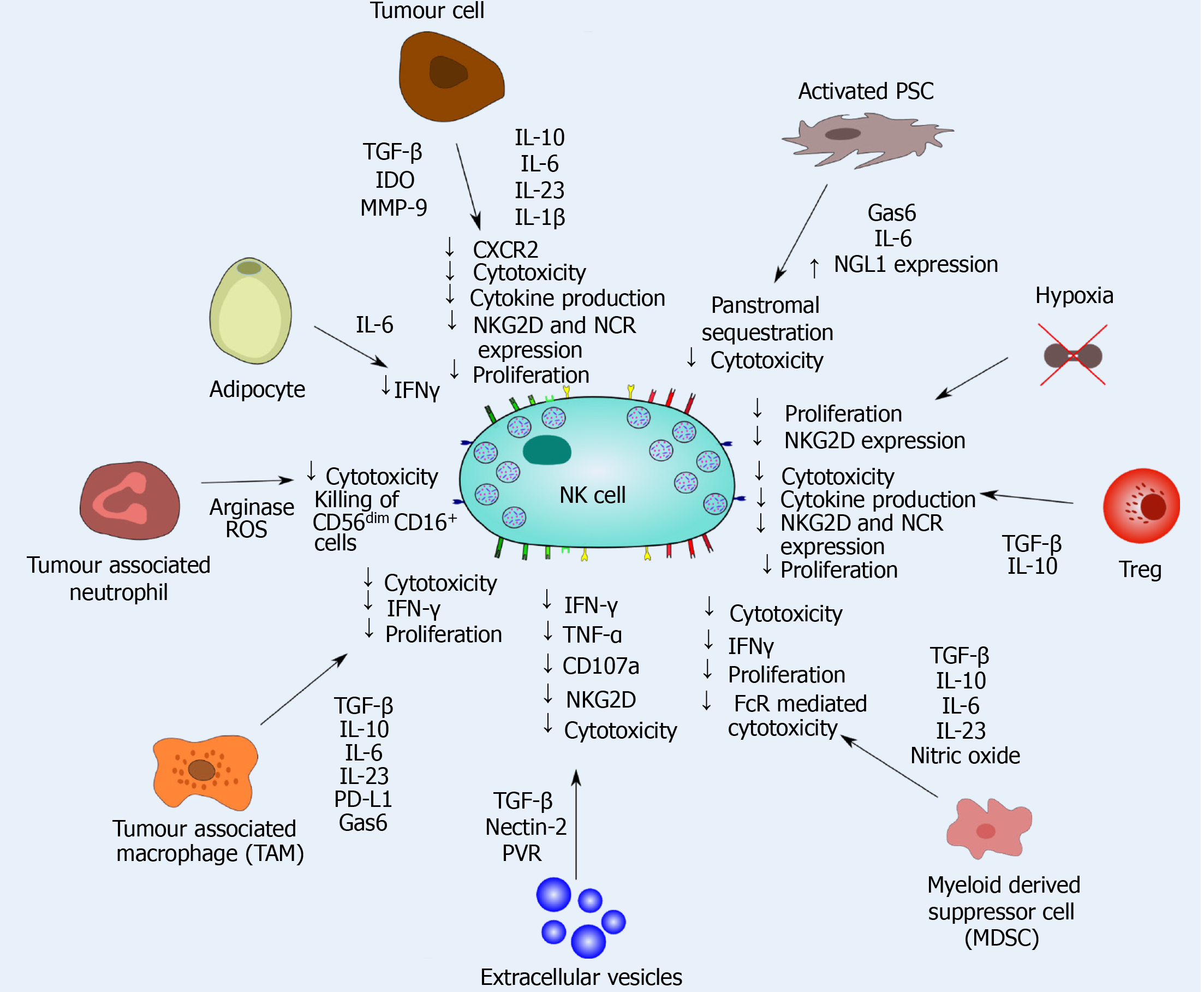
NK cell-stromal cell interactions have been shown to result in significant cellular dysfunction and exclusion of NK cells from tumour tissues, suggesting that NK cells can be educated by the TME[47,63]. As crucial players in the development of the pre-metastatic niche, extracellular vesicles are key to the progression of PDAC and contain large numbers of immune regulatory factors including TGF-β, nectin-2 and PVR. Flow cytometric analysis following in vitro co-culture of NK cells and extracellular vesicles demonstrated downregulation of multiple NK cell receptors and cytokines, specifically, IFN-γ, TNFα, CD107a and NKG2D, resulting in gross cytotoxic impairment (demonstrated through tumour sphere cytotoxicity assays) and NK cell dysfunction. This impairment was further associated with the activation of the TGF-β- Smad3/4 signalling pathway[64]. It should also be noted that NK cell dysfunction is heavily regulated by the soluble factors and cytokines secreted by both tumoural and stromal cells, with TGF-β, IDO, MMPs and interleukins proving largely responsible for this impairment (Figure 5)[50,60,65-67].
NK cell interaction with suppressive immunoregulatory cells has a significant impact on cytotoxic effector function. Both MDSCs and TAMs produce IL-23, IL-6, IL10 and TGF-β which results in the downregulation of IFN-γ, perforin and IL-12 production by NK cells, decreasing cytotoxicity and NK cell proliferation within the TME[65]. TAMs also inhibit NK cell function through cell-cell interactions. M2 macrophages express PDL-1 which binds to PD-1 expressed on NK cells. This checkpoint protein prevents NK cell engagement and induces downregulation of the activating receptors NKG2D, natural cytotoxicity receptors and DNAM1, leading to reduced cytotoxicity[67]. Immunosuppressive Tregs release IL-10 and TGF-β into the TME. This cytokine release decreases NK cell cytotoxicity through the downregulation of activating receptors and decreased production of anti-tumour cytokines such as IFN-γ[65].
Moreover, MDSCs have also been shown to augment FcR mediate NK cell functions. Adoptive transfer of MDSC in a Panc02-EGFR+ murine model of pancreatic cancer significantly inhibited the efficacy of monoclonal antibody therapy, with mice receiving Cetuximab + MDSCs expressing significantly larger tumour volumes than did mice treated with Cetuximab + splenocytes. Furthermore, NK cells co-cultured with tumour derived (melanoma) MDSCs were found to express significantly reduced phospho-ERK than did though cultured alone (as measured by flow cytometry). Thus, it was concluded that MDSCs inhibit FcR mediated signal transduction, resulting in impaired cytokine production, ADCC dysfunction and reduced anti-tumour activity. An effect that was found to be, at least in part, in response to MDSC nitric oxide production[68].
Likewise, tumour-associated neutrophils have been shown to impair NK cell function through the release of arginase and ROS[67]. In vitro co-culture assays using PBMCs derived from healthy donors demonstrated that activated granulocytes (stimulated with Phorbol 12-myristate 13-acetate) produced ROS including hydrogen peroxide, which was found to be cytotoxic to CD56dim CD16+ NK cells, but not CD56brightCD16- subsets, suggesting that interactions with stromal cells may result in differential effects on cytotoxic effector subset[69].
Tumour-associated macrophages and cancer-associated fibroblasts have also been shown to produce growth arrest-specific gene 6 (Gas6) in the pancreatic TME. As a negative regulator of the immune system, the Gas6-AXL pathway is seen to prevent NK cell activation. Orthotopic syngeneic models of pancreatic cancer in which tumour cells derived from KPC mice were transduced with zsGreen/Luciferase and orthotopically injected into the pancreas of immune-compromised mice were used to investigate the role of Gas6 in NK cell activation and pancreatic cancer development. Pharmacological blockade of Gas6 signalling using neutralising antibodies was found to inhibit pancreatic cancer metastasis. Moreover, immunohistochemical analysis of NK cell infiltrates revealed a significant increase in the number of NKp46+ NK cells in lung metastasis in mice treated with anti-Gas6 therapy when compared to the control. This finding was also observed in the tumour draining lymph nodes; however no significant difference was observed in NK cell infiltration in primary tumour sites between treatment groups[70]. As such, Gas6 blockade may prove a promising new therapeutic target for the treatment of metastatic lesions in pancreatic cancer.
NK cells have been shown to be excluded from tumour tissue as a result of NK-stromal cell interactions. Through ex vivo immunostaining and Ariol image analysis of tissue micro-arrays, Ene-Obong et al[4] demonstrated that infiltrates of CD56+ natural killer cells were significantly lower in the juxtatumoural compartment of PDAC tissues (stage I-III) when compared to panstroma. This finding suggests PSCs sequester NK cells in the panstromal compartment of the TME, preventing NK induced cancer cell death. Similarly, Lim et al[50] demonstrated that NK cell frequencies in malignant tissue from PDAC patients (stage I-IV) were as low as < 0.5% (as assessed by flow cytometry). This low infiltration was attributed to reduced expression of the CXCR2 receptor on NK cells which resulted in poor chemotaxis into tumour tissues.
Known orchestrators of the TME, pancreatic stellate cells are crucial regulators of immune cell infiltrates in pancreatic cancer and have been shown to promote tumour progression through the development of an immunosuppressive environment[5,71-73]. In an orthotopic mouse model of pancreatic cancer in which either Panc02 cells alone or in combination with activated PSCs were injected into the pancreas of C57BL/6 mice, Li et al[74] report a significant reduction in the number of NK cells in tumour tissue in mice co-transplanted with PSCs when compared to mice injected with Panc02 cells alone. This finding is consistent with ex vivo analysis of human PDAC samples[4]. Further work is needed to demonstrate the mechanistic link between PSCs and NK cell tumoural exclusion.
In a recent study, Francescone et al[75] demonstrated dynamic crosstalk between PDAC cancer cells, CAFs and immune cells. Specifically, in in vitro co-culture assays CAFs were found to ectopically express the neural presynaptic protein NetrinG1 (NG1) whilst its binding partner, NGL1 was identified on PDAC cells. This interaction was found to convey protection on cancer cells from NK cell-driven elimination,a fact quantified through CRISPR/Cas9 NG1 knockout which resulted in decreased expression of the immunosuppressive cytokines TGF-β, IL-8 and IL-6, and restored NK cell anti-tumour activation. This finding was reproduced in murine orthotopic models of PDAC in which NGL1 was knocked out of syngeneic mouse cells. This work provides a potential novel target in PDAC in which the immunosuppressive nature of PDAC induce by CAF cells can be reverted.
Finally, in vitro and xenograft models of PDAC in NOD SCID mice demonstrated that stromal TGF-β signalling stimulates CAF cells to secrete IL-6, which in turn suppresses NK cell function as assessed through NK cell killing assays. Concomitantly, stromal TGF-β limits NK cell function itself[76]. In vivo TGFβ blockade using the anti-mouse TGFβR2 mAb, 2G8, was found to reduce tumour progression, an effect that was reversed upon NK cell depletion[76]. Furthermore, a conditional KRAS (G12D) model of pancreatic cancer combined with a high-fat calorie diet demonstrated that stromal adipocytes produce IL-6, reducing NK cell function through IL-6 mediated downregulation of IFN-γ production. Thus, it has been suggested that adipocytes and PSCs may provide tumour sanctuaries within the TME through the immunosuppression of NK cells[77,78].
Taken together these findings demonstrate the complex interactions between NK cells and the PDAC microenvironment. Despite their cytotoxic efficacy against malignancy, the dysfunction induced by stromal cells greatly augments the natural anti-tumoral activity of NK cells. As such, a deeper understanding of these interactions is crucial to fully unlock the potential of NK cells in the treatment of PDAC.
Despite the known dysfunction of NK cells associated with PDAC, these cytotoxic effector units display evident cytotoxic capabilities and as such have received much attention as a potential immunotherapeutic tool in the treatment of PDAC. One of the immunotherapeutic routes explored is the use of NK cells as cellular immunotherapy[79]. When compared to T cells, the use of NK cells as cellular immune-therapeutics express several advantages. Firstly, NK cells present a much lower risk of on-target/off-tumour toxicity, rendering NK cells a relatively safe treatment option. Moreover, neurotoxicity, cytokine release syndrome and graft-versus-host disease are much less likely to occur in chimeric antigen receptor (CAR)-NK treatment than observed with the use of CAR-T therapy. Secondly, due to this reduced risk of graft-versus-host disease from allogenic NK sources, NK cells have the potential to be derived from multiple sources, including cell lines such as NK92. This facilitates the development of a truly ‘off-the-shelf’ cellular immunotherapeutic, eliminating the need for personalised therapeutics and the subsequent challenges these treatments invoke[79]. Thirdly, CAR-NK cells retain their natural cytotoxic capabilities and consequently can eliminate malignant cells in both a CAR dependent and independent manner[79,80].
Several studies have focused on harnessing the anti-tumoral efficacy of NK cells against PDAC. Lee et al[81], rationally designed a CAR-NK to specifically target folate receptor alpha (FRα) and death receptor 4 (DR4) which were found to be highly expressed on tumour cells. In addition, the CAR-NK was loaded with an apoptosis-inducing death ligand to further induce anti-tumoral cytotoxicity. Treatment with the FRα/DR4 targeting NK cells significantly increased tumour-selective apoptosis and NK cell infiltration in tumour tissue in sub-cutaneous models of pancreatic cancer. Similarly, Xia et al[82] investigated the efficacy of a Robo1 bi-specific CAR-NK cell treatment in combination with 125I seed radiotherapy in orthotopic murine models of pancreatic cancer. Expressed on pancreatic cancer cells, Robo-1 is a member of the axon guidance receptor family which has been found modulate T-cell chemotaxis into the TME. Tumour size was significantly reduced in mice treated with combination therapy when compared to 125I seed treatment alone. Moreover, tumours of mice receiving combination therapy displayed a significantly higher greyscale value than did 125I treatment alone. Thus, it was concluded that bi-specific CAR-NK cells may prove a promising immunotherapeutic when combined with 125I seed therapy in treatment of pancreatic cancer. Identification of novel antigens for therapy are useful strategies for cell-based therapy[83,84].
In addition to CAR therapies, cytokine supplement either alone or in combination with additional therapeutics has demonstrated significant benefit in both preclinical studies and clinical trials. In combination with the immune priming CD40 agonist, supplementation of IL-15 in orthotopic and KPC mouse models of pancreatic cancer resulted in a significant increase in immune cell infiltration into tumour tissue (assessed through multi-colour flow cytometry), particularly of NK and CD8+ T cells. This infiltration resulted in enhanced anti-tumour effect and significantly improved long term survival (log-rank tests; P ≤ 0.0001)[85]. Furthermore, Lin et al[86] demonstrated that allogeneic NK cell transfer in combination with irreversible electroporation significantly increased median progression-free and overall survival in stage III PDAC patients and increased median overall survival in stage IV patients. Moreover, multiple allogenic transfers correlated with better prognosis in stage III patients. Similarly, treatment with a dendritic cell/cytokine-induced killer cell vaccine was found increase both overall and progression-free survival in advanced pancreatic cancer patients[87]. Taken together these results highlight the therapeutic potential of NK cell-based therapies. Current clinical trials employing NK cell therapy in pancreatic cancer (identified through entering the search terms ‘natural killer cells’ and ‘pan
| Primary therapy | Additional intervention | Tumour type | Phase | NCT number | Status | Ref. |
| NK cell infusions | Irreversible electroporation | Advanced pancreatic cancer | I/II | NCT02718859 | Completed | [90,91] |
| Dendritic cell activated, cytokine induced killer treatment | S-1 (drug) | Advanced pancreatic cancer | I/II | NCT01781520 | Completed | [87,92] |
| BiCAR NK cells (ROBO1 CAR-NK cells) | Pancreatic cancer | I/II | NCT03941457 | Recruiting | [93] | |
| Ex-vivo expanded autologous NK cells (SNK01) | Trastuzumab; Cetuximab | Advanced solid tumour; metastatic cancer; HER-2+ breast cancer; HER-2 positive gastric cancer; HER-2 protein overexpression; oesophageal cancer; ovarian cancer; endometrium cancer; bladder cancer; pancreatic cancer; colorectal cancer; NSCLC; EGFR+ NSCLC; head and neck squamous cell carcinoma; triple-negative breast cancer; cervical cancer; sarcoma | I/IIa | NCT04464967 | Not yet recruiting | [94] |
| High activity NK cells | Pancreatic cancer | I/II | NCT03008304 | Completed | [95] | |
| Activated NK cells | Lung cancer; breast cancer; colon cancer; pancreatic cancer; ovarian cancer | I/II | NCT03634501 | Recruiting | [96] | |
| FT500-an allogenic, iPSC derived NK cell immunotherapy | Nivolumab; pembrolizumab; atezolizumab; cyclophosphamide; fludarabine; IL-2 | Advanced solid tumours; lymphoma; gastric cancer; colorectal cancer; head and neck cancer; squamous cell carcinoma; EGFR positive solid tumour; HER2 positive breast cancer; hepatocellular carcinoma; small-cell lung cancer; renal cell carcinoma; pancreas cancer; melanoma; NSCLC; urothelial carcinoma, cervical cancer; microsatellite instability; merkel cell carcinoma | I | NCT03841110 | Recruiting | [97] |
| FT500-101 allogenic NK cell immunotherapy | Advanced solid tumours; lymphoma; gastric cancer; colorectal cancer; head and neck cancer; squamous cell carcinoma; EGFR positive solid tumour; HER2 positive breast cancer; hepatocellular carcinoma; small-cell lung cancer; renal cell carcinoma; pancreas cancer; melanoma; NSCLC; urothelial carcinoma, cervical cancer; microsatellite instability; merkel cell carcinoma | Observational study | NCT04106167 | Recruiting | [98] | |
| FATE-NK100 (donor-derived ex-vivo activated immunotherapy) | Trastuzumab; Cetuximab | HER2+ gastric cancer; colorectal cancer; head and neck squamous cell carcinoma; EGFR+ solid tumours; advanced solid tumours; HER2 postie breast cancer; hepatocellular carcinoma; NSCLC; renal cell carcinoma; pancreatic cancer; melanoma | I | NCT03319459 | Active, not recruiting | [99] |
| Autologous dendritic cell vaccine loaded with personalised peptides to stimulate innate and adaptive immune response via activating T and NK cells | Standard of care; Nivolumab | Pancreatic adenocarcinoma | Ib | NCT04627246 | Recruiting | [100] |
| ACE1702 cellular therapy (anti-HER2 NK cells) | Cyclophosphamide; Fludarabine | Locally advanced solid tumours; metastatic cancer; solid tumour; HER-2+ gastric cancer; HER-2 + metastatic breast cancer | I | NCT04319757 | Recruiting | [101] |
| NK cells | Bortezomib | CML; pancreatic cancer; colon/rectal cancer; multiple myeloma; carcinoma-NSCLC | I | NCT00720785 | Recruiting | [102] |
| Cytokine-induced killer cells | Tegafur; Gimeracil; Oteracil potassium | Advanced cancer | II | NCT03002831 | Terminated | [103,104] |
| Anti-MUC1 CAR-pNK cells | Hepatocellular carcinoma; NSCLC; pancreatic cancer; triple negative invasive breast carcinoma; malignant glioma of the brain; colorectal carcinoma; gastric carcinoma | I/II | NCT02839954 | Unknown | [105] | |
| Autologous NK/NK T cell immunotherapy | Breast cancer; glioma; hepatocellular carcinoma; squamous cell lung cancer; pancreatic cancer; colon cancer; prostate cancer | I | NCT00909558 | Suspended | [106] |
NK cells are powerful effector units, which, when harnessed, can confer striking therapeutic benefit. With the innate effector units demonstrating strong efficacy against malignancy, both in preclinical studies, and clinical trials, the potential for NK cell therapy in PDAC is only just beginning to come to light. Additional research is needed to fully elucidate the role of NK cells in pancreatic cancer and deconvolute the intricate relationships between NK and stromal cells within the TME, facilitating co-targeting of tumour stroma[73,88]. Through defining these relationships, novel functional and mechanistic insights into this devastating disease can be achieved[89] and the full therapeutic potential of NK cells can be harnessed.
Manuscript source: Invited manuscript
Specialty type: Oncology
Country/Territory of origin: United Kingdom
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gao DJ S-Editor: Zhang H L-Editor: A P-Editor: Wang LL
| 1. | Neuzillet C, Rousseau B, Kocher H, Bourget P, Tournigand C. Unravelling the pharmacologic opportunities and future directions for targeted therapies in gastro-intestinal cancers Part 1: GI carcinomas. Pharmacol Ther. 2017;174:145-172. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 2. | Rahib L, Smith BD, Aizenberg R, Rosenzweig AB, Fleshman JM, Matrisian LM. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res. 2014;74:2913-2921. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3888] [Cited by in F6Publishing: 4585] [Article Influence: 458.5] [Reference Citation Analysis (0)] |
| 3. | Young K, Hughes DJ, Cunningham D, Starling N. Immunotherapy and pancreatic cancer: unique challenges and potential opportunities. Ther Adv Med Oncol. 2018;10:1758835918816281. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 40] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 4. | Ene-Obong A, Clear AJ, Watt J, Wang J, Fatah R, Riches JC, Marshall JF, Chin-Aleong J, Chelala C, Gribben JG, Ramsay AG, Kocher HM. Activated pancreatic stellate cells sequester CD8+ T cells to reduce their infiltration of the juxtatumoral compartment of pancreatic ductal adenocarcinoma. Gastroenterology. 2013;145:1121-1132. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 340] [Cited by in F6Publishing: 384] [Article Influence: 34.9] [Reference Citation Analysis (0)] |
| 5. | Froeling FE, Kocher HM. Homeostatic restoration of desmoplastic stroma rather than its ablation slows pancreatic cancer progression. Gastroenterology. 2015;148:849-850. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 6. | Ren B, Cui M, Yang G, Wang H, Feng M, You L, Zhao Y. Tumor microenvironment participates in metastasis of pancreatic cancer. Mol Cancer. 2018;17:108. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 182] [Cited by in F6Publishing: 314] [Article Influence: 52.3] [Reference Citation Analysis (0)] |
| 7. | Uzunparmak B, Sahin IH. Pancreatic cancer microenvironment: a current dilemma. Clin Transl Med. 2019;8:2. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 62] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 8. | Di Maggio F, Arumugam P, Delvecchio FR, Batista S, Lechertier T, Hodivala-Dilke K, Kocher HM. Pancreatic stellate cells regulate blood vessel density in the stroma of pancreatic ductal adenocarcinoma. Pancreatology. 2016;16:995-1004. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 51] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 9. | Trovato R, Fiore A, Sartori S, Canè S, Giugno R, Cascione L, Paiella S, Salvia R, De Sanctis F, Poffe O, Anselmi C, Hofer F, Sartoris S, Piro G, Carbone C, Corbo V, Lawlor R, Solito S, Pinton L, Mandruzzato S, Bassi C, Scarpa A, Bronte V, Ugel S. Immunosuppression by monocytic myeloid-derived suppressor cells in patients with pancreatic ductal carcinoma is orchestrated by STAT3. J Immunother Cancer. 2019;7:255. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 90] [Cited by in F6Publishing: 108] [Article Influence: 21.6] [Reference Citation Analysis (0)] |
| 10. | Principe DR, DeCant B, Mascariñas E, Wayne EA, Diaz AM, Akagi N, Hwang R, Pasche B, Dawson DW, Fang D, Bentrem DJ, Munshi HG, Jung B, Grippo PJ. TGFβ Signaling in the Pancreatic Tumor Microenvironment Promotes Fibrosis and Immune Evasion to Facilitate Tumorigenesis. Cancer Res. 2016;76:2525-2539. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 109] [Cited by in F6Publishing: 141] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 11. | Xu JY, Wang WS, Zhou J, Liu CY, Shi JL, Lu PH, Ding JL. The Importance of a Conjoint Analysis of Tumor-Associated Macrophages and Immune Checkpoints in Pancreatic Cancer. Pancreas. 2019;48:904-912. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 12. | Tesfaye AA, Kamgar M, Azmi A, Philip PA. The evolution into personalized therapies in pancreatic ductal adenocarcinoma: challenges and opportunities. Expert Rev Anticancer Ther. 2018;18:131-148. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 13. | Gonzalez-Rodriguez AP, Villa-Álvarez M, Sordo-Bahamonde C, Lorenzo-Herrero S, Gonzalez S. NK Cells in the Treatment of Hematological Malignancies. J Clin Med. 2019;8. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 14. | Granzin M, Wagner J, Köhl U, Cerwenka A, Huppert V, Ullrich E. Shaping of Natural Killer Cell Antitumor Activity by Ex Vivo Cultivation. Front Immunol. 2017;8:458. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 93] [Cited by in F6Publishing: 113] [Article Influence: 16.1] [Reference Citation Analysis (1)] |
| 15. | Kumar S. Natural killer cell cytotoxicity and its regulation by inhibitory receptors. Immunology. 2018;154:383-393. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 93] [Cited by in F6Publishing: 125] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 16. | Mehta RS, Randolph B, Daher M, Rezvani K. NK cell therapy for hematologic malignancies. Int J Hematol. 2018;107:262-270. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 51] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 17. | Urlaub D, Höfer K, Müller ML, Watzl C. LFA-1 Activation in NK Cells and Their Subsets: Influence of Receptors, Maturation, and Cytokine Stimulation. J Immunol. 2017;198:1944-1951. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 60] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 18. | Seidel UJ, Schlegel P, Lang P. Natural killer cell mediated antibody-dependent cellular cytotoxicity in tumor immunotherapy with therapeutic antibodies. Front Immunol. 2013;4:76. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 153] [Cited by in F6Publishing: 167] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 19. | Lefort CT, Ley K. Neutrophil arrest by LFA-1 activation. Front Immunol. 2012;3:157. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 93] [Cited by in F6Publishing: 97] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 20. | Yuki K, Bu W, Xi J, Sen M, Shimaoka M, Eckenhoff RG. Isoflurane binds and stabilizes a closed conformation of the leukocyte function-associated antigen-1. FASEB J. 26:4408-4417. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 37] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 21. | Zhang M, March ME, Lane WS, Long EO. A signaling network stimulated by β2 integrin promotes the polarization of lytic granules in cytotoxic cells. Sci Signal. 2014;7:ra96. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 51] [Cited by in F6Publishing: 53] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 22. | Chaldakov GN. Colchicine, Inflammation and Fibrosis in Cardiovascular Disease: Merging Three Classical Tales. Bulgarian Society for Cell Biology. 2017;28:105-110. [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 23. | Paul S, Lal G. The Molecular Mechanism of Natural Killer Cells Function and Its Importance in Cancer Immunotherapy. Front Immunol. 2017;8:1124. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 276] [Cited by in F6Publishing: 414] [Article Influence: 59.1] [Reference Citation Analysis (0)] |
| 24. | Mentlik AN, Sanborn KB, Holzbaur EL, Orange JS. Rapid lytic granule convergence to the MTOC in natural killer cells is dependent on dynein but not cytolytic commitment. Mol Biol Cell. 2010;21:2241-2256. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 107] [Cited by in F6Publishing: 119] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 25. | Mukherjee M, Mace EM, Carisey AF, Ahmed N, Orange JS. Quantitative Imaging Approaches to Study the CAR Immunological Synapse. Mol Ther. 2017;25:1757-1768. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 42] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 26. | Viswanath DI, Mace EM, Hsu HT, Orange JS. Quantification of natural killer cell polarization and visualization of synaptic granule externalization by imaging flow cytometry. Clin Immunol. 2017;177:70-75. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 27. | Brown AC, Dobbie IM, Alakoskela JM, Davis I, Davis DM. Super-resolution imaging of remodeled synaptic actin reveals different synergies between NK cell receptors and integrins. Blood. 2012;120:3729-3240. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 47] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 28. | Mace EM, Dongre P, Hsu HT, Sinha P, James AM, Mann SS, Forbes LR, Watkin LB, Orange JS. Cell biological steps and checkpoints in accessing NK cell cytotoxicity. Immunol Cell Biol. 2014;92:245-255. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 131] [Cited by in F6Publishing: 133] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 29. | Stinchcombe JC, Salio M, Cerundolo V, Pende D, Arico M, Griffiths GM. Centriole polarisation to the immunological synapse directs secretion from cytolytic cells of both the innate and adaptive immune systems. BMC Biol. 2011;9:45. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 52] [Cited by in F6Publishing: 55] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 30. | Abarca-Rojano E, Muñiz-Hernández S, Moreno-Altamirano MM, Mondragón-Flores R, Enriquez-Rincón F, Sánchez-García FJ. Re-organization of mitochondria at the NK cell immune synapse. Immunol Lett. 2009;122:18-25. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 50] [Cited by in F6Publishing: 51] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 31. | Capuano C, Paolini R, Molfetta R, Frati L, Santoni A, Galandrini R. PIP2-dependent regulation of Munc13-4 endocytic recycling: impact on the cytolytic secretory pathway. Blood. 2012;119:2252-2262. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 32. | Backes CS, Friedmann KS, Mang S, Knörck A, Hoth M, Kummerow C. Natural killer cells induce distinct modes of cancer cell death: Discrimination, quantification, and modulation of apoptosis, necrosis, and mixed forms. J Biol Chem. 2018;293:16348-16363. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 58] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 33. | Zhu Y, Huang B, Shi J. Fas ligand and lytic granule differentially control cytotoxic dynamics of natural killer cell against cancer target. Oncotarget. 2016;7:47163-47172. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 45] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 34. | Allen F, Bobanga ID, Rauhe P, Barkauskas D, Teich N, Tong C, Myers J, Huang AY. CCL3 augments tumor rejection and enhances CD8+ T cell infiltration through NK and CD103+ dendritic cell recruitment via IFNγ. Oncoimmunology. 2017;7:e1393598. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 57] [Cited by in F6Publishing: 51] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 35. | Mishra HK, Pore N, Michelotti EF, Walcheck B. Anti-ADAM17 monoclonal antibody MEDI3622 increases IFNγ production by human NK cells in the presence of antibody-bound tumor cells. Cancer Immunol Immunother. 2018;67:1407-1416. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 31] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 36. | Wu SY, Fu T, Jiang YZ, Shao ZM. Natural killer cells in cancer biology and therapy. Mol Cancer. 2020;19:120. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 330] [Cited by in F6Publishing: 279] [Article Influence: 69.8] [Reference Citation Analysis (0)] |
| 37. | Chiossone L, Dumas PY, Vienne M, Vivier E. Natural killer cells and other innate lymphoid cells in cancer. Nat Rev Immunol. 2018;18:671-688. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 463] [Cited by in F6Publishing: 607] [Article Influence: 121.4] [Reference Citation Analysis (0)] |
| 38. | Trinchieri G. Biology of natural killer cells. Adv Immunol. 1989;47:187-376. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2111] [Cited by in F6Publishing: 2137] [Article Influence: 61.1] [Reference Citation Analysis (0)] |
| 39. | Sun C, Xu J, Huang Q, Huang M, Wen H, Zhang C, Wang J, Song J, Zheng M, Sun H, Wei H, Xiao W, Sun R, Tian Z. High NKG2A expression contributes to NK cell exhaustion and predicts a poor prognosis of patients with liver cancer. Oncoimmunology. 2016;6:e1264562. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 131] [Cited by in F6Publishing: 168] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 40. | Huang Y, Chen Z, Jang JH, Baig MS, Bertolet G, Schroeder C, Huang S, Hu Q, Zhao Y, Lewis DE, Qin L, Zhu MX, Liu D. PD-1 blocks lytic granule polarization with concomitant impairment of integrin outside-in signaling in the natural killer cell immunological synapse. J Allergy Clin Immunol 2018; 142: 1311-1321. e8. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 41. | Liu Y, Cheng Y, Xu Y, Wang Z, Du X, Li C, Peng J, Gao L, Liang X, Ma C. Increased expression of programmed cell death protein 1 on NK cells inhibits NK-cell-mediated anti-tumor function and indicates poor prognosis in digestive cancers. Oncogene. 2017;36:6143-6153. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 206] [Cited by in F6Publishing: 227] [Article Influence: 32.4] [Reference Citation Analysis (0)] |
| 42. | Pasero C, Gravis G, Granjeaud S, Guerin M, Thomassin-Piana J, Rocchi P, Salem N, Walz J, Moretta A, Olive D. Highly effective NK cells are associated with good prognosis in patients with metastatic prostate cancer. Oncotarget. 2015;6:14360-14373. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 116] [Cited by in F6Publishing: 145] [Article Influence: 18.1] [Reference Citation Analysis (0)] |
| 43. | Kamei R, Yoshimura K, Yoshino S, Inoue M, Asao T, Fuse M, Wada S, Kuramasu A, Furuya-Kondo T, Oga A, Iizuka N, Suzuki N, Maeda N, Watanabe Y, Matsukuma S, Iida M, Takeda S, Ueno T, Yamamoto N, Fukagawa T, Katai H, Sasaki H, Hazama S, Oka M, Nagano H. Expression levels of UL16 binding protein 1 and natural killer group 2 member D affect overall survival in patients with gastric cancer following gastrectomy. Oncol Lett. 2018;15:747-754. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 44. | Hoshikawa M, Aoki T, Matsushita H, Karasaki T, Hosoi A, Odaira K, Fujieda N, Kobayashi Y, Kambara K, Ohara O, Arita J, Hasegawa K, Kakimi K, Kokudo N. NK cell and IFN signatures are positive prognostic biomarkers for resectable pancreatic cancer. Biochem Biophys Res Commun. 2018;495:2058-2065. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 45. | Paolini R, Bernardini G, Molfetta R, Santoni A. NK cells and interferons. Cytokine Growth Factor Rev. 2015;26:113-120. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 84] [Cited by in F6Publishing: 93] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 46. | Lee AJ, Ashkar AA. The Dual Nature of Type I and Type II Interferons. Front Immunol. 2018;9:2061. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 296] [Cited by in F6Publishing: 390] [Article Influence: 65.0] [Reference Citation Analysis (0)] |
| 47. | Yang C, Cheng H, Zhang Y, Fan K, Luo G, Fan Z, Huang Q, Lu Y, Jin K, Wang Z, Yu X, Liu C. Anergic natural killer cells educated by tumor cells are associated with a poor prognosis in patients with advanced pancreatic ductal adenocarcinoma. Cancer Immunol Immunother. 2018;67:1815-1823. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 48. | Brooks J, Fleischmann-Mundt B, Woller N, Niemann J, Ribback S, Peters K, Demir IE, Armbrecht N, Ceyhan GO, Manns MP, Wirth TC, Kubicka S, Bernhardt G, Smyth MJ, Calvisi DF, Gürlevik E, Kühnel F. Perioperative, Spatiotemporally Coordinated Activation of T and NK Cells Prevents Recurrence of Pancreatic Cancer. Cancer Res. 2018;78:475-488. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 51] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 49. | Hu S, Yang J, Shangguan J, Eresen A, Li Y, Ma Q, Yaghmai V, Velichko Y, Hu C, Zhang Z. Natural killer cell-based adoptive transfer immunotherapy for pancreatic ductal adenocarcinoma in a KrasLSL-G12Dp53LSL-R172HPdx1-Cre mouse model. Am J Cancer Res. 2019;9:1757-1765. [PubMed] [Cited in This Article: ] |
| 50. | Lim SA, Kim J, Jeon S, Shin MH, Kwon J, Kim TJ, Im K, Han Y, Kwon W, Kim SW, Yee C, Kim SJ, Jang JY, Lee KM. Defective Localization With Impaired Tumor Cytotoxicity Contributes to the Immune Escape of NK Cells in Pancreatic Cancer Patients. Front Immunol. 2019;10:496. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 44] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 51. | Ames E, Canter RJ, Grossenbacher SK, Mac S, Chen M, Smith RC, Hagino T, Perez-Cunningham J, Sckisel GD, Urayama S, Monjazeb AM, Fragoso RC, Sayers TJ, Murphy WJ. NK Cells Preferentially Target Tumor Cells with a Cancer Stem Cell Phenotype. J Immunol. 2015;195:4010-4019. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 127] [Cited by in F6Publishing: 154] [Article Influence: 17.1] [Reference Citation Analysis (0)] |
| 52. | Muthalagu N, Monteverde T, Raffo-Iraolagoitia X, Wiesheu R, Whyte D, Hedley A, Laing S, Kruspig B, Upstill-Goddard R, Shaw R, Neidler S, Rink C, Karim SA, Gyuraszova K, Nixon C, Clark W, Biankin AV, Carlin LM, Coffelt SB, Sansom OJ, Morton JP, Murphy DJ. Repression of the Type I Interferon Pathway Underlies MYC- and KRAS-Dependent Evasion of NK and B Cells in Pancreatic Ductal Adenocarcinoma. Cancer Discov. 2020;10:872-887. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 96] [Cited by in F6Publishing: 76] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 53. | Ponath V, Frech M, Bittermann M, Al Khayer R, Neubauer A, Brendel C, Pogge von Strandmann E. The Oncoprotein SKI Acts as A Suppressor of NK Cell-Mediated Immunosurveillance in PDAC. Cancers (Basel). 2020;12. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 54. | Van Audenaerde JRM, Roeyen G, Darcy PK, Kershaw MH, Peeters M, Smits ELJ. Natural killer cells and their therapeutic role in pancreatic cancer: A systematic review. Pharmacol Ther. 2018;189:31-44. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 55. | Ostapchuk YO, Perfilyeva YV, Kali A, Tleulieva R, Yurikova OY, Stanbekova GE, Karalnik BV, Belyaev NN. Fc Receptor is Involved in Nk Cell Functional Anergy Induced by Miapaca2 Tumor Cell Line. Immunol Invest. 2020;1-16. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 56. | Duan Q, Li H, Gao C, Zhao H, Wu S, Wu H, Wang C, Shen Q, Yin T. High glucose promotes pancreatic cancer cells to escape from immune surveillance via AMPK-Bmi1-GATA2-MICA/B pathway. J Exp Clin Cancer Res. 2019;38:192. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 57. | Ou ZL, Luo Z, Wei W, Liang S, Gao TL, Lu YB. Hypoxia-induced shedding of MICA and HIF1A-mediated immune escape of pancreatic cancer cells from NK cells: role of circ_0000977/miR-153 axis. RNA Biol. 2019;16:1592-1603. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 75] [Cited by in F6Publishing: 113] [Article Influence: 22.6] [Reference Citation Analysis (0)] |
| 58. | Peng YP, Xi CH, Zhu Y, Yin LD, Wei JS, Zhang JJ, Liu XC, Guo S, Fu Y, Miao Y. Altered expression of CD226 and CD96 on natural killer cells in patients with pancreatic cancer. Oncotarget. 2016;7:66586-66594. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 48] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 59. | Van Audenaerde JRM, De Waele J, Marcq E, Van Loenhout J, Lion E, Van den Bergh JMJ, Jesenofsky R, Masamune A, Roeyen G, Pauwels P, Lardon F, Peeters M, Smits ELJ. Interleukin-15 stimulates natural killer cell-mediated killing of both human pancreatic cancer and stellate cells. Oncotarget. 2017;8:56968-56979. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 42] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 60. | Peng YP, Zhang JJ, Liang WB, Tu M, Lu ZP, Wei JS, Jiang KR, Gao WT, Wu JL, Xu ZK, Miao Y, Zhu Y. Elevation of MMP-9 and IDO induced by pancreatic cancer cells mediates natural killer cell dysfunction. BMC Cancer. 2014;14:738. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 58] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 61. | Peng YP, Zhu Y, Zhang JJ, Xu ZK, Qian ZY, Dai CC, Jiang KR, Wu JL, Gao WT, Li Q, Du Q, Miao Y. Comprehensive analysis of the percentage of surface receptors and cytotoxic granules positive natural killer cells in patients with pancreatic cancer, gastric cancer, and colorectal cancer. J Transl Med. 2013;11:262. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 94] [Cited by in F6Publishing: 113] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 62. | Jun E, Song AY, Choi JW, Lee HH, Kim MY, Ko DH, Kang HJ, Kim SW, Bryceson Y, Kim SC, Kim HS. Progressive Impairment of NK Cell Cytotoxic Degranulation Is Associated With TGF-β1 Deregulation and Disease Progression in Pancreatic Cancer. Front Immunol. 2019;10:1354. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 63. | Barrow AD, Colonna M. Tailoring Natural Killer cell immunotherapy to the tumour microenvironment. Semin Immunol. 2017;31:30-36. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 64. | Zhao J, Schlößer HA, Wang Z, Qin J, Li J, Popp F, Popp MC, Alakus H, Chon SH, Hansen HP, Neiss WF, Jauch KW, Bruns CJ, Zhao Y. Tumor-Derived Extracellular Vesicles Inhibit Natural Killer Cell Function in Pancreatic Cancer. Cancers (Basel). 2019;11. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 54] [Cited by in F6Publishing: 82] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 65. | Konjević GM, Vuletić AM, Mirjačić Martinović KM, Larsen AK, Jurišić VB. The role of cytokines in the regulation of NK cells in the tumor environment. Cytokine. 2019;117:30-40. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 89] [Cited by in F6Publishing: 142] [Article Influence: 28.4] [Reference Citation Analysis (0)] |
| 66. | Ostrand-Rosenberg S, Sinha P, Beury DW, Clements VK. Cross-talk between myeloid-derived suppressor cells (MDSC), macrophages, and dendritic cells enhances tumor-induced immune suppression. Semin Cancer Biol. 2012;22:275-281. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 362] [Cited by in F6Publishing: 404] [Article Influence: 33.7] [Reference Citation Analysis (0)] |
| 67. | Bassani B, Baci D, Gallazzi M, Poggi A, Bruno A, Mortara L. Natural Killer Cells as Key Players of Tumor Progression and Angiogenesis: Old and Novel Tools to Divert Their Pro-Tumor Activities into Potent Anti-Tumor Effects. Cancers (Basel). 2019;11:461. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 89] [Cited by in F6Publishing: 94] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 68. | Stiff A, Trikha P, Mundy-Bosse B, McMichael E, Mace TA, Benner B, Kendra K, Campbell A, Gautam S, Abood D, Landi I, Hsu V, Duggan M, Wesolowski R, Old M, Howard JH, Yu L, Stasik N, Olencki T, Muthusamy N, Tridandapani S, Byrd JC, Caligiuri M, Carson WE. Nitric Oxide Production by Myeloid-Derived Suppressor Cells Plays a Role in Impairing Fc Receptor-Mediated Natural Killer Cell Function. Clin Cancer Res. 2018;24:1891-1904. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 115] [Cited by in F6Publishing: 157] [Article Influence: 26.2] [Reference Citation Analysis (0)] |
| 69. | Harlin H, Hanson M, Johansson CC, Sakurai D, Poschke I, Norell H, Malmberg KJ, Kiessling R. The CD16- CD56(bright) NK cell subset is resistant to reactive oxygen species produced by activated granulocytes and has higher antioxidative capacity than the CD16+ CD56(dim) subset. J Immunol. 2007;179:4513-4519. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 61] [Cited by in F6Publishing: 63] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 70. | Ireland L, Luckett T, Schmid MC, Mielgo A. Blockade of Stromal Gas6 Alters Cancer Cell Plasticity, Activates NK Cells, and Inhibits Pancreatic Cancer Metastasis. Front Immunol. 2020;11:297. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 71. | Kadaba R, Birke H, Wang J, Hooper S, Andl CD, Di Maggio F, Soylu E, Ghallab M, Bor D, Froeling FE, Bhattacharya S, Rustgi AK, Sahai E, Chelala C, Sasieni P, Kocher HM. Imbalance of desmoplastic stromal cell numbers drives aggressive cancer processes. J Pathol. 2013;230:107-117. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 98] [Cited by in F6Publishing: 128] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 72. | Froeling FE, Feig C, Chelala C, Dobson R, Mein CE, Tuveson DA, Clevers H, Hart IR, Kocher HM. Retinoic acid-induced pancreatic stellate cell quiescence reduces paracrine Wnt-β-catenin signaling to slow tumor progression. Gastroenterology 2011; 141: 1486-1497, 1497.e1-1497. 14;. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 251] [Cited by in F6Publishing: 314] [Article Influence: 24.2] [Reference Citation Analysis (0)] |
| 73. | Neuzillet C, Tijeras-Raballand A, Ragulan C, Cros J, Patil Y, Martinet M, Erkan M, Kleeff J, Wilson J, Apte M, Tosolini M, Wilson AS, Delvecchio FR, Bousquet C, Paradis V, Hammel P, Sadanandam A, Kocher HM. Inter- and intra-tumoural heterogeneity in cancer-associated fibroblasts of human pancreatic ductal adenocarcinoma. J Pathol. 2019;248:51-65. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 152] [Cited by in F6Publishing: 183] [Article Influence: 36.6] [Reference Citation Analysis (0)] |
| 74. | Li C, Cui L, Yang L, Wang B, Zhuo Y, Zhang L, Wang X, Zhang Q, Zhang S. Pancreatic Stellate Cells Promote Tumor Progression by Promoting an Immunosuppressive Microenvironment in Murine Models of Pancreatic Cancer. Pancreas. 2020;49:120-127. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 29] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 75. | Francescone R, Vendramini-Costa DB, Franco-Barraza J, Wagner J, Muir A, Gabitova L, Pazina T, Luong T, Shah N, Rollins D, Malik R, Gupta S, Thapa R, Restifo D, Lau A, Zhou Y, Cai KQ, Hensley HH, Nicolas E, Kruger WD, Devarajan K, Balachandran S, El-Deiry WS, Heiden MV, Campbell K, Astsaturov I, Cukierman E. Abstract 2038: NG1/NGL1 engagement supports PDAC development via CAF to PDAC nutrition and CAF-regulated immunosuppression. Cancer Research. 2019;79 (13 Supplement):2038. [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 76. | Huang H, Zhang Y, Gallegos V, Sorrelle N, Zaid MM, Toombs J, Du W, Wright S, Hagopian M, Wang Z, Hosein AN, Sathe AA, Xing C, Koay EJ, Driscoll KE, Brekken RA. Targeting TGFβR2-mutant tumors exposes vulnerabilities to stromal TGFβ blockade in pancreatic cancer. EMBO Mol Med. 2019;11:e10515. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 44] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 77. | Jewett A, Kos J, Fong Y, Ko MW, Safaei T, Perišić Nanut M, Kaur K. NK cells shape pancreatic and oral tumor microenvironments; role in inhibition of tumor growth and metastasis. Semin Cancer Biol. 2018;53:178-188. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 44] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 78. | Kaur K, Chang HH, Topchyan P, Cook JM, Barkhordarian A, Eibl G, Jewett A. Deficiencies in Natural Killer Cell Numbers, Expansion, and Function at the Pre-Neoplastic Stage of Pancreatic Cancer by KRAS Mutation in the Pancreas of Obese Mice. Front Immunol. 2018;9:1229. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 79. | Xie G, Dong H, Liang Y, Ham JD, Rizwan R, Chen J. CAR-NK cells: A promising cellular immunotherapy for cancer. EBioMedicine. 2020;59:102975. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 219] [Cited by in F6Publishing: 390] [Article Influence: 97.5] [Reference Citation Analysis (0)] |
| 80. | Oei VYS, Siernicka M, Graczyk-Jarzynka A, Hoel HJ, Yang W, Palacios D, Almåsbak H, Bajor M, Clement D, Brandt L, Önfelt B, Goodridge J, Winiarska M, Zagozdzon R, Olweus J, Kyte JA, Malmberg KJ. Intrinsic Functional Potential of NK-Cell Subsets Constrains Retargeting Driven by Chimeric Antigen Receptors. Cancer Immunol Res. 2018;6:467-480. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 56] [Cited by in F6Publishing: 57] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 81. | Lee YE, Ju A, Choi HW, Kim JC, Kim EE, Kim TS, Kang HJ, Kim SY, Jang JY, Ku JL, Kim SC, Jun E, Jang M. Rationally designed redirection of natural killer cells anchoring a cytotoxic ligand for pancreatic cancer treatment. J Control Release. 2020;326:310-323. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 23] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 82. | Xia N, Haopeng P, Gong JU, Lu J, Chen Z, Zheng Y, Wang Z, Sun YU, Yang Z, Hoffman RM, Liu F. Robo1-specific CAR-NK Immunotherapy Enhances Efficacy of 125I Seed Brachytherapy in an Orthotopic Mouse Model of Human Pancreatic Carcinoma. Anticancer Res. 2019;39:5919-5925. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 83. | Raj D, Nikolaidi M, Garces I, Lorizio D, Castro NM, Caiafa SG, Moore K, Brown NF, Kocher HM, Duan X, Nelson BH, Lemoine NR, Marshall JF. CEACAM7 Is an Effective Target for CAR T-cell Therapy of Pancreatic Ductal Adenocarcinoma. Clin Cancer Res. 2021;27:1538-1552. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 31] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 84. | Raj D, Yang MH, Rodgers D, Hampton EN, Begum J, Mustafa A, Lorizio D, Garces I, Propper D, Kench JG, Kocher HM, Young TS, Aicher A, Heeschen C. Switchable CAR-T cells mediate remission in metastatic pancreatic ductal adenocarcinoma. Gut. 2019;68:1052-1064. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 80] [Cited by in F6Publishing: 90] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 85. | Van Audenaerde JR, Marcq E, von Scheidt B, Davey AS, Oliver AJ, De Waele J, Quatannens D, Van Loenhout J, Pauwels P, Roeyen G, Lardon F, Slaney CY, Peeters M, Kershaw MH, Darcy PK, Smits EL. Novel combination immunotherapy for pancreatic cancer: potent anti-tumor effects with CD40 agonist and interleukin-15 treatment. Clin Transl Immunology. 2020;9:e1165. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 86. | Lin M, Alnaggar M, Liang S, Wang X, Liang Y, Zhang M, Chen J, Niu L, Xu K. An important discovery on combination of irreversible electroporation and allogeneic natural killer cell immunotherapy for unresectable pancreatic cancer. Oncotarget. 2017;8:101795-101807. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 87. | Jiang N, Qiao G, Wang X, Morse MA, Gwin WR, Zhou L, Song Y, Zhao Y, Chen F, Zhou X, Huang L, Hobeika A, Yi X, Xia X, Guan Y, Song J, Ren J, Lyerly HK. Dendritic Cell/Cytokine-Induced Killer Cell Immunotherapy Combined with S-1 in Patients with Advanced Pancreatic Cancer: A Prospective Study. Clin Cancer Res. 2017;23:5066-5073. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 51] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 88. | Kocher HM, Basu B, Froeling FEM, Sarker D, Slater S, Carlin D, deSouza NM, De Paepe KN, Goulart MR, Hughes C, Imrali A, Roberts R, Pawula M, Houghton R, Lawrence C, Yogeswaran Y, Mousa K, Coetzee C, Sasieni P, Prendergast A, Propper DJ. Phase I clinical trial repurposing all-trans retinoic acid as a stromal targeting agent for pancreatic cancer. Nat Commun. 2020;11:4841. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 125] [Cited by in F6Publishing: 106] [Article Influence: 26.5] [Reference Citation Analysis (0)] |
| 89. | Sivapalan L, Kocher HM, Ross-Adams H, Chelala C. Molecular profiling of ctDNA in pancreatic cancer: Opportunities and challenges for clinical application. Pancreatology. 2021;21:363-378. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 90. | Niu L. Combination of Irreversible Electroporation and NK Immunotherapy for Advanced Pancreatic Cancer [accessed 27 Jan 2021]. In: ClinicalTrials.gov [Internet]. Bethesda (MD): U.S. National Library of Medicine. Available from: http://clinicaltrials.gov/show/NCT02718859 ClinicalTrials.gov Identifier: NCT0271885987. [Cited in This Article: ] |
| 91. | Lin M, Liang S, Wang X, Liang Y, Zhang M, Chen J, Niu L, Xu K. Percutaneous irreversible electroporation combined with allogeneic natural killer cell immunotherapy for patients with unresectable (stage III/IV) pancreatic cancer: a promising treatment. J Cancer Res Clin Oncol. 2017;143:2607-2618. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 36] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 92. | Jiang N. Study of S-1 Plus DC-CIK for Patients With Unresectable Locally Advanced Pancreatic Cancer [accessed 27 Jan 2021]. In: ClinicalTrials.gov [Internet]. Bethesda (MD): U.S. National Library of Medicine. Available from: http://clinicaltrials.gov/show/NCT01781520 ClinicalTrials.gov Identifier: NCT01781520. [Cited in This Article: ] |
| 93. | Wang Z. Clinical Research of ROBO1 Specific BiCAR-NK Cells on Patients With Pancreatic Cancer Cancer. [accessed 27 Jan 2021]. In: ClinicalTrials.gov [Internet]. Bethesda (MD): U.S. National Library of Medicine. Available from: http://clinicaltrials.gov/show/NCT03941457 ClinicalTrials.gov Identifier: NCT03941457. [Cited in This Article: ] |
| 94. | Song P. Safety and Preliminary Efficacy of SNK01 in Combination With Trastuzumab or Cetuximab in Subjects With Advanced HER2 or EGFR Cancers Cancer. [accessed 27 Jan 2021]. In: ClinicalTrials.gov [Internet]. Bethesda (MD): U.S. National Library of Medicine. Available from: http://clinicaltrials.gov/show/NCT04464967 ClinicalTrials.gov Identifier: NCT04464967. [Cited in This Article: ] |
| 95. | Fuda-Cancer-Hospital. High-activity Natural Killer Immunotherapy for Small Metastases of Pancreatic Cancer. [accessed 27 Jan 2021]. In: ClinicalTrials.gov [Internet]. Bethesda (MD): U.S. National Library of Medicine. Available from: http://clinicaltrials.gov/show/NCT03008304 ClinicalTrials.gov Identifier: NCT03008304. [Cited in This Article: ] |
| 96. | Chen Z. Clinical Study on Anti-tumor Effect Induced by Activated Primary Natural Killer (NK) Cells. [accessed 27 Jan 2021]. In: ClinicalTrials.gov [Internet]. Bethesda (MD): U.S. National Library of Medicine. Available from: http://clinicaltrials.gov/show/NCT03634501 ClinicalTrials.gov Identifier: NCT03634501. [Cited in This Article: ] |
| 97. | Chou J. FT500 as Monotherapy and in Combination With Immune Checkpoint Inhibitors in Subjects With Advanced Solid Tumors Cancer. [accessed 27 Jan 2021]. In: ClinicalTrials.gov [Internet]. Bethesda (MD): U.S. National Library of Medicine. Available from: http://clinicaltrials.gov/show/NCT03841110 ClinicalTrials.gov Identifier: NCT03841110. [Cited in This Article: ] |
| 98. | Chu W. Long-term, Non-interventional, Observational Study Following Treatment With Fate Therapeutics FT500 Cellular Immunotherapy. [accessed 27 Jan 2021]. In: ClinicalTrials.gov [Internet]. Bethesda (MD): U.S. National Library of Medicine. Available from: http://clinicaltrials.gov/show/NCT04106167 ClinicalTrials.gov Identifier: NCT04106167. [Cited in This Article: ] |
| 99. | Cooley S. FATE-NK100 as Monotherapy and in Combination With Monoclonal Antibody in Subjects With Advanced Solid Tumors. [accessed 27 Jan 2021]. In: ClinicalTrials.gov [Internet]. Bethesda (MD): U.S. National Library of Medicine. Available from: http://clinicaltrials.gov/show/NCT03319459 ClinicalTrials.gov Identifier: NCT03319459. [Cited in This Article: ] |
| 100. | Digklia A. Personalized Vaccine With SOC Chemo Followed by Nivo in Pancreatic Cancer. [accessed 27 Jan 2021]. In: ClinicalTrials.gov [Internet]. Bethesda (MD): U.S. National Library of Medicine. Available from: http://clinicaltrials.gov/show/NCT04627246 ClinicalTrials.gov Identifier: NCT04627246. [Cited in This Article: ] |
| 101. | Kurman M. ACE1702 in Subjects With Advanced or Metastatic HER2-expressing Solid Tumors. [accessed 27 Jan 2021]. In: ClinicalTrials.gov [Internet]. Bethesda (MD): U.S. National Library of Medicine. Available from: http://clinicaltrials.gov/show/NCT04319757 ClinicalTrials.gov Identifier: NCT04319757. [Cited in This Article: ] |
| 102. | Childs R. Natural Killer Cells and Bortezomib to Treat Cancer Cancer. [accessed 27 Jan 2021]. In: ClinicalTrials.gov [Internet]. Bethesda (MD): U.S. National Library of Medicine. Available from: http://clinicaltrials.gov/show/NCT00720785 ClinicalTrials.gov Identifier: NCT00720785. [Cited in This Article: ] |
| 103. | Wang Z, Liu Y, Li R, Shang Y, Zhang Y, Zhao L, Li W, Yang Y, Zhang X, Yang T, Nie C, Han F, Luo S, Gao Q, Song Y. Autologous cytokine-induced killer cell transfusion increases overall survival in advanced pancreatic cancer. J Hematol Oncol. 2016;9:6. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 104. | Gao Q. Autologous Cytokine-induced Killer Cells Combined Chemotherapy in Advanced Pancreatic Cancer. [accessed 27 Jan 2021]. In: ClinicalTrials.gov [Internet]. Bethesda (MD): U.S. National Library of Medicine. Available from: http://clinicaltrials.gov/show/NCT03002831 ClinicalTrials.gov Identifier: NCT03002831. [Cited in This Article: ] |
| 105. | Yang L. CAR-pNK Cell Immunotherapy in MUC1 Positive Relapsed or Refractory Solid Tumor Cancer. [accessed 27 Jan 2021]. In: ClinicalTrials.gov [Internet]. Bethesda (MD): U.S. National Library of Medicine. Available from: http://clinicaltrials.gov/show/NCT02839954 ClinicalTrials.gov Identifier: NCT02839954. [Cited in This Article: ] |
| 106. | Korn D. Safety and Effectiveness Study of Autologous Natural Killer and Natural Killer T Cells on Cancer. [accessed 27 Jan 2021]. In: ClinicalTrials.gov [Internet]. Bethesda (MD): U.S. National Library of Medicine. Available from: http://clinicaltrials.gov/show/NCT00909558 ClinicalTrials.gov Identifier: NCT00909558. [Cited in This Article: ] |