- Neurosurgery Unit, Highly Specialized Hospital and of National Importance “Garibaldi,” Piazza Santa Maria di Gesù 5, Catania, Italy,
- Department of Neurosurgery, Cannizzaro Hospital, Via Messina 829, Catania, Italy.
Correspondence Address:
Gianluca Scalia
Neurosurgery Unit, Highly Specialized Hospital and of National Importance “Garibaldi,” Piazza Santa Maria di Gesù 5, Catania, Italy,
DOI:10.25259/SNI_365_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Giovanni Federico Nicoletti1, Giuseppe Emmanuele Umana2, Francesca Graziano1, Alessandro Calì1, Marco Fricia2, Salvatore Cicero2, Gianluca Scalia1. Cauda equina syndrome caused by lumbar leptomeningeal metastases from lung adenocarcinoma mimicking a schwannoma. 01-Aug-2020;11:225
How to cite this URL: Giovanni Federico Nicoletti1, Giuseppe Emmanuele Umana2, Francesca Graziano1, Alessandro Calì1, Marco Fricia2, Salvatore Cicero2, Gianluca Scalia1. Cauda equina syndrome caused by lumbar leptomeningeal metastases from lung adenocarcinoma mimicking a schwannoma. 01-Aug-2020;11:225. Available from: https://surgicalneurologyint.com/surgicalint-articles/10180/
Abstract
Background: Cauda equina syndromes (CESs) due to leptomeningeal metastases from primitive lung tumors are rare. Despite recent advancements in neuro-oncology and molecular biology, the prognosis for these patients remains poor. Here, we present a case in which a patient developed lumbar leptomeningeal metastases from lung carcinoma that contributed to a CES and reviewed the appropriate literature.
Case Description: A 55-year-old female presented with the left lower extremity sciatica/weakness. Two years ago, a then 53-year-old female had received Gamma Knife stereotactic radiosurgery (SRS) for a cerebellopontine angle schwannoma. Recently, she underwent resection of lung carcinoma and SRS for a right hemispheric cerebellar metastasis. Now at age 55, she presented with the left lower extremity sciatica/weakness. When her new lumbar MR was interpreted as showing a L5 schwannoma, a L4-L5 laminectomy was performed at surgery, the authors encountered multifocal leptomeningeal metastases densely infiltrating the cauda equina. Although only subtotal resection/decompression of tumor was feasible, she did well for the ensuing year. The histological diagnosis confirmed the lesion to be a poorly differentiated lung adenocarcinoma.
Conclusion: Patients with a history of prior metastatic lung cancer may present with spinal leptomeningeal metastases resulting in a CES.
Keywords: Metastases, Schwannoma, Leptomeningeal, Cauda equina, Lung cancer
INTRODUCTION
Neoplasms that cause a cauda equina syndrome (CES) can be either primary or secondary lesions. The primary tumors include myxopapillary ependymomas, neurinomas, and more rarely, paragangliomas, astrocytomas, chordomas, and giant cell tumors. Secondary metastatic tumors, including leptomeningeal metastases, are typically attributed to the following primary cancers: lung, breast, renal, colon, and lymphoma.[
METHODS
Fourteen articles from PubMed, Scopus, and Google Scholar databases (Mesh terms: cauda equina AND metastases AND lung carcinoma OR spinal AND leptomeningeal AND metastases AND lung carcinoma) focused on lung leptomeningeal metastases resulting in CES.[
CASE DESCRIPTION
History
Two years ago, the patient had received Gamma Knife stereotactic radiosurgery (SRS) for a right cerebellopontine angle schwannoma. She recently had undergone resection of a lung adenocarcinoma and had received SRS for a right hemispheric cerebellar metastasis (e.g., infiltrating roof of the IV ventricle). She now presented at age 55 with the left lower extremity sciatica, and a partial CES characterized by a left L5-sided partial foot drop (4/5 level), left L5 sensory changes, and severe saddle hypoesthesia.
MR study
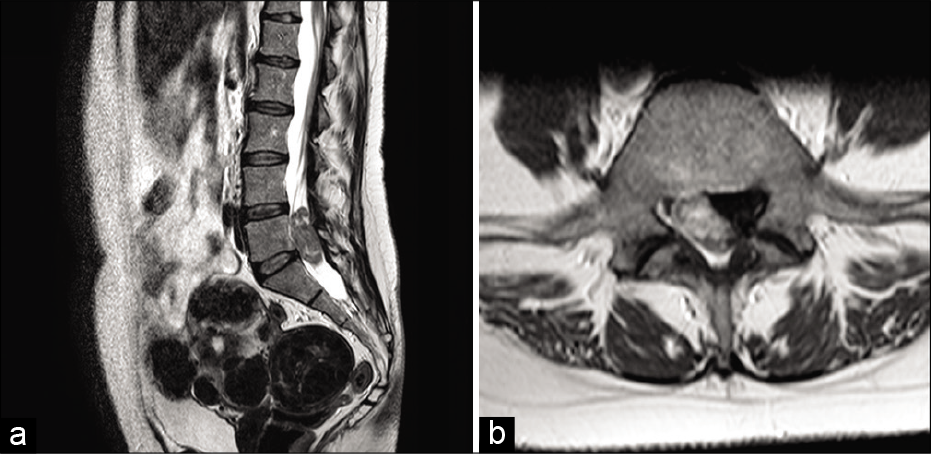
The lumbosacral MR was interpreted as a schwannoma of the cauda equina at the L5 level; no additional lesions were found when MR was utilized to evaluate the rest of the neuraxis [
Surgery and histology
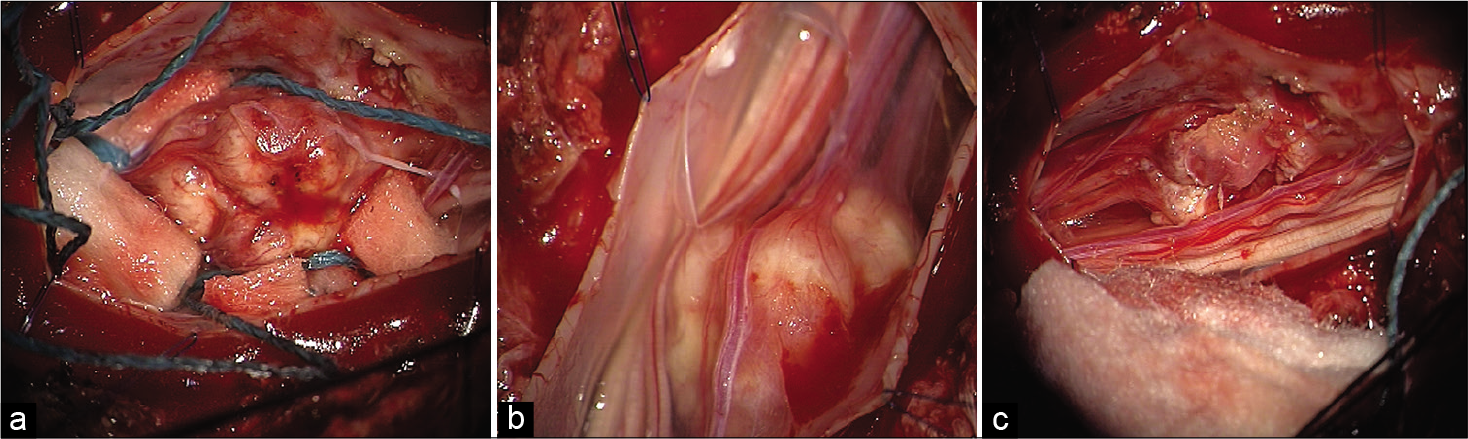
An L4-L5 laminectomy was performed, and only subtotal resection of tumor was feasible as multiple leptomeningeal metastases were densely adherent to/and infiltrated the multiple nerve roots of the cauda equina [
Figure 2:
Intraoperative images showing exposure of the lesion after dural opening. (a) A good exposure showed the relationships between the neoplasia and the roots of the cauda equina, whose limits did not appear completely distinct. (b) A subtotal excision of the neoplasm has been achieved, with radicular sparing (c).
Postoperative course
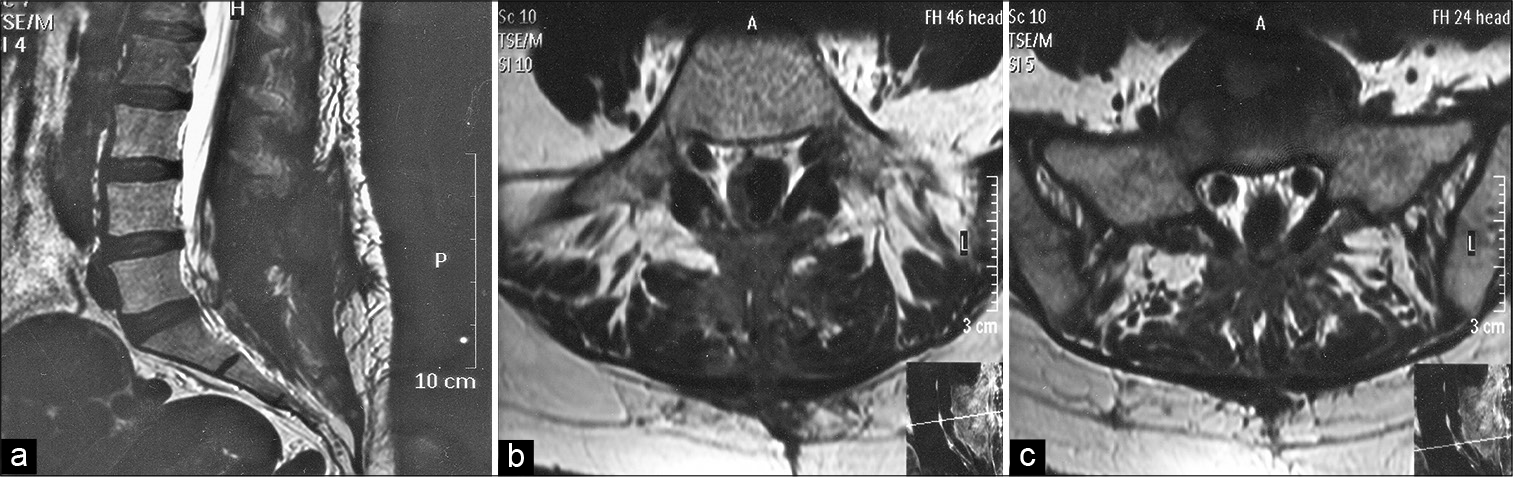
Postoperatively, her prior symptoms/signs improved, and she was discharged on adjuvant chemotherapy and radiotherapy. One-month later, the lumbosacral magnetic resonance imaging confirmed adequate spinal canal decompression at the L4-L5 level (e.g., subtotal removal) [
DISCUSSION
Vertebral or paravertebral metastases develop in 50% of patients with breast or lung cancer and carry poor prognoses.[
Leptomeningeal carcinomatosis
Notably, leptomeningeal carcinomatosis carries a median survival of just 1.3 months without adequate adjuvant therapy.[
CONCLUSION
Lung carcinoma with leptomeningeal metastases involving nerve roots of the cauda equina is extremely rare and carries a poor prognosis. Surgery should be performed to confirm the pathological diagnosis or, if the pathology is already known, to provide pain relief and/or alleviation of neurological symptoms/signs, even if it does not prolong overall survival.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Alicioglu B, Saynak M. Spinal leptomeningeal metastasis in a patient with squamous cell lung cancer. Rev Port Pneumol. 2008. 14: 875-9
2. Ampil FL, Caldito G, Heldmann M. Palliation and survival in metastatic tumors compressing the cauda equina: A 19-year radiotherapeutic experience. J Palliat Med. 2003. 6: 33-6
3. Chamberlain MC, Kormanik P. Carcinoma meningitis secondary to non-small cell lung cancer: Combined modality therapy. Arch Neurol. 1998. 55: 506-12
4. Fraser S, Roberts L, Murphy E. Cauda equina syndrome: A literature review of its definition and clinical presentation. Arch Phys Med Rehabil. 2009. 90: 1964-8
5. Gwak HS, Joo J, Kim S, Yoo H, Shin SH, Han JY. Analysis of treatment outcomes of intraventricular chemotherapy in 105 patients for leptomeningeal carcinomatosis from non-small-cell lung cancer. J Thorac Oncol. 2013. 8: 599-605
6. Kotil K, Kilinc BM, Bilge T. Spinal metastasis of occult lung carcinoma causing cauda equina syndrome. J Clin Neurosci. 2007. 14: 372-5
7. Le Rhun E, Taillibert S, Chamberlain MC. Carcinomatous meningitis: Leptomeningeal metastases in solid tumors. Surg Neurol Int. 2013. 4: S265-88
8. Leviov M, Dale J, Stein M, Ben-Shahar M, Ben-Arush M, Milstein D. The management of metastatic spinal cord compression: A radiotherapeutic success ceiling. Int J Radiat Oncol Biol Phys. 1993. 27: 231-4
9. Lin CL, Chang JL, Lo HC, Wu KA. Extramedullary-intradural spinal metastasis of small cell lung cancer causing cauda equina syndrome. Am J Med Sci. 2010. 339: 192-4
10. Liu Y, Wang B, Qian Y, Di D, Wang M, Zhang X. Cauda equine syndrome as the primary symptom of leptomeningeal metastases from lung cancer: A case report and review of literature. Onco Targets Ther. 2018. 11: 5009-13
11. Löhr M, Tzouras G, Kocher M, Stenzel W, Reithmeier T, Klug N. Treatment strategies of space-occupying intradural metastases of the cauda equina of nonneurogenic origin. Acta Neurochir (Wien). 2009. 151: 207-15
12. Okamoto H, Shinkai T, Matsuno Y, Saijo N. Intradural parenchymal involvement in the spinal subarachnoid space associated with primary lung cancer. Cancer. 1993. 72: 2583-8
13. Sakai M, Ishikawa S, Ito H, Ozawa Y, Yamamoto T, Onizuka M. Carcinomatous meningitis from non-small-cell lung cancer responding to gefitinib. Int J Clin Oncol. 2006. 11: 243-5
14. Tsimpas A, Post NH, Moshel Y, Frempong-Boadu AK. Large cell neuroendocrine carcinoma of the lung metastatic to the cauda equina. Spine J. 2010. 10: e1-5
15. Walid MS, Ajjan M, Johnston KW, Robinson JS. Cauda equina syndrome-think of cancer. Perm J. 2008. 12: 48-51
16. Xiong J, Zhang P. Cauda equina syndrome caused by isolated spinal extramedullary-intradural cauda equina metastasis is the primary symptom of small cell lung cancer: A case report and review of the literature. Int J Clin Exp Med. 2015. 8: 10044-50