Abstract
Background
Steady progress in outcomes has been observed after standard treatment by surgery and chemotherapy in patients with advanced ovarian cancer (AOC), but little is known about outcomes after alternative neoadjuvant chemotherapy (NAC) proposed to primary inoperable patients. We assessed whether NAC offers comparable survival to standard treatment, whether survival rates have progressed over time, and what the optimal extent of surgery at late interval debulking surgery (IDS) should be.
Methods
This was a retrospective data analysis of prospectively recorded patients with poor prognosis AOC treated by platinum/taxane NAC and late IDS (after six cycles). Independent prognostic factors for surgical morbidity and overall survival (OS) are determined and survival outcomes are compared to survival rates for a similar group of patients treated with platinum protocols.
Results
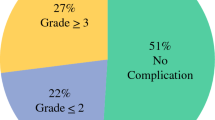
A total of 118 patients with stages IIIC-IV AOC (median age: 64 years, stage IV: 31 %) received IDS (46 % standard surgery and 54 % radical, with 68 % obtaining complete resection). Major morbidity was 18 %. OS was 42 months across all patients (95 % confidence interval 35.3–49.1) and 80 months in stage IIIC. This is higher by 15 months than after platinum-based treatment. Higher morbidity was associated with bowel resection. Longer OS was associated with ASA class I, stage IIIC, no bowel surgery, and no residual disease.
Conclusions
The neoadjuvant approach with late IDS offers survival similar to that reported by standard treatment, with progress in outcomes compared with rates after platinum treatment. The goal of IDS surgery is complete resection, while sparing surrounding organs.

Similar content being viewed by others
References
Stoeckle E, Paravis P, Floquet A, et al. Number of residual nodules, better than size, defines optimal surgery in advanced epithelial ovarian cancer. Int J Gynecol Cancer. 2004;14:779–87.
du Bois A, Quinn M, Thigpen T, et al. 2004. Consensus statements on the management of ovarian cancer: final document of the 3rd International Gynecologic Cancer Intergroup Ovarian Cancer Consensus Conference (GCIG OCCC 2004). Ann Oncol. 2005;16(Suppl 8):viii7-12.
Eisenkop SM, Spirtos NM, Lin WC. “Optimal” cytoreduction for advanced epithelial ovarian cancer: a commentary. Gynecol Oncol. 2006;103:329–35.
Peiretti M, Zanagnolo V, Aletti GD, et al. Role of maximal primary cytoreductive surgery in patients with advanced epithelial ovarian and tubal cancer: surgical and oncological outcomes. Single institution experience. Gynecol Oncol. 2010;119:259–64.
Heintz APM OF, Maisonneuve P, Quinn MA, et al. FIGO Annual Report 26. Carcinoma of the ovary. Int J Gynecol Cancer. 2009.
Elattar A, Bryant A, Winter-Roach BA, et al. Optimal primary surgical treatment for advanced epithelial ovarian cancer. Cochrane Database Syst Rev 2011;CD007565.
Chi DS, Eisenhauer EL, Zivanovic O, et al. Improved progression-free and overall survival in advanced ovarian cancer as a result of a change in surgical paradigm. Gynecol Oncol. 2009;114:26-31.
Harter P, Muallem ZM, Buhrmann C, et al. Impact of a structured quality management program on surgical outcome in primary advanced ovarian cancer. Gynecol Oncol. 2011;121:615-9.
Vergote I, Trope CG, Amant F, et al. Neoadjuvant chemotherapy or primary surgery in stage IIIC or IV ovarian cancer. N Engl J Med. 2010;363:943-53.
Sehouli J, Savvatis K, Braicu EI, et al. Primary versus interval debulking surgery in advanced ovarian cancer: results from a systematic single-center analysis. Int J Gynecol Cancer. 2010;20:1331-40.
Chi DS, Musa F, Dao F, et al. An analysis of patients with bulky advanced stage ovarian, tubal, and peritoneal carcinoma treated with primary debulking surgery (PDS) during an identical time period as the randomized EORTC-NCIC trial of PDS vs neoadjuvant chemotherapy (NACT). Gynecol Oncol. 2012;124:10-4.
Bristow RE, Chi DS. Platinum-based neoadjuvant chemotherapy and interval surgical cytoreduction for advanced ovarian cancer: a meta-analysis. Gynecol Oncol. 2006;103:1070-6.
du Bois A, Marth C, Pfisterer J, et al. Neoadjuvant chemotherapy cannot be regarded as adequate routine therapy strategy of advanced ovarian cancer. Int J Gynecol Cancer. 2012;22:182-5.
Stoeckle E, Boubli B, Floquet A, et al. Optimal timing of interval debulking surgery in advanced ovarian cancer: yet to be defined? Eur J Obstet Gynecol Reprod Biol. 2011;159:407-12.
Schwartz PE, Rutherford TJ, Chambers JT, et al. Neoadjuvant chemotherapy for advanced ovarian cancer: long-term survival. Gynecol Oncol. 1999;72:93-9.
Winter WE, 3rd, Maxwell GL, Tian C, et al. Prognostic factors for stage III epithelial ovarian cancer: a Gynecologic Oncology Group Study. J Clin Oncol. 2007;25:3621-7.
du Bois A, Reuss A, Pujade-Lauraine E, et al. Role of surgical outcome as prognostic factor in advanced epithelial ovarian cancer: a combined exploratory analysis of 3 prospectively randomized phase 3 multicenter trials: by the Arbeitsgemeinschaft Gynaekologische Onkologie Studiengruppe Ovarialkarzinom (AGO-OVAR) and the Groupe d’Investigateurs Nationaux Pour les Etudes des Cancers de l’Ovaire (GINECO). Cancer. 2009;115:1234-44.
Le T, Shahriari P, Hopkins L, et al. Prognostic significance of tumor necrosis in ovarian cancer patients treated with neoadjuvant chemotherapy and interval surgical debulking. Int J Gynecol Cancer. 2006;16:986–90.
Hou J, Kelly M, Yu H, et al. Neoadjuvant chemotherapy lessens surgical morbidity in advanced ovarian cancer and leads to improved survival in stage IV disease. Gynecol Oncol. 2007;105:211-7.
Kang S, Nam B-H. Does Neoadjuvant chemotherapy increase optimal cytoreduction rate in advanced ovarian cancer? Meta-analysis of 21 studies. Ann Surg Oncol. 2009;16:2315-20.
Gerestein CG, Damhuis RA, Burger CW, Kooi GS. Postoperative mortality after primary cytoreductive surgery for advanced stage epithelial ovarian cancer: a systematic review. Gynecol Oncol. 2009;114:523-7.
Wright JD, Lewin SN, Deutsch I et al. Defining the limits of radical cytoreductive surgery for ovarian cancer. Gynecol Oncol. 2011;123:467-73.
Aletti GD, Dowdy SC, Podratz KC, Cliby WA. Relationship among surgical complexity, short-term morbidity, and overall survival in primary surgery for advanced ovarian cancer. Am J Obstet Gynecol. 2007;197:676 e671-7.
Matsuo K, Prather CP, Ahn EH, et al. Significance of perioperative infection in survival of patients with ovarian cancer. Int J Gynecol Cancer. 2012;22:245–53.
Houvenaeghel G, Gutowski M, Butarelli M, et al. Modified posterior pelvic exenteration for ovarian cancer. Int J Gynecol Cancer. 2009;19:968-73.
Kalogera E, Dowdy SC, Mariani A, et al. Multiple large bowel resection: potential risk factor for anastomotic leak. Gynecol Oncol. 2013. doi:10.1016/j.ygyno.2013.04.002.
Lim MC, Song YJ, Seo SS et al. Residual cancer stem cells after interval cytoreductive surgery following neoadjuvant chemotherapy could result in poor treatment outcomes for ovarian cancer. Onkologie. 2010;33:324–30.
Acknowledgment
The authors gratefully acknowledge medical writing assistance from Pippa McKelvie-Sebileau, employee of Institut Bergonié.
Conflict of interest
The authors have no conflicts of interest to declare. This work was not supported by any external financial support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stoeckle, E., Bourdarias, L., Guyon, F. et al. Progress in Survival Outcomes in Patients with Advanced Ovarian Cancer Treated by Neo-Adjuvant Platinum/Taxane-Based Chemotherapy and Late Interval Debulking Surgery. Ann Surg Oncol 21, 629–636 (2014). https://doi.org/10.1245/s10434-013-3278-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-013-3278-x