Abstract
Background
Ampullary carcinomas typically have either intestinal or pancreatobiliary type of differentiation, histopathologically resembling carcinomas of its adjacent tissues (duodenum, bile duct, or pancreas). We evaluated whether the histologic type itself is more important for long-term survival than the fact that the tumor originated in the ampulla.
Methods
Microscopic slides from 207 consecutive pancreatoduodenectomies were reviewed (72 pancreatic, 46 biliary, 61 ampullary, and 28 duodenal adenocarcinomas; 76 intestinal type, 131 pancreatobiliary type). Tumor size, nodal involvement, margin involvement, degree of differentiation, vascular involvement, and perineural growth, as well as overall survival, were compared between different origins of the same histologic type.
Results
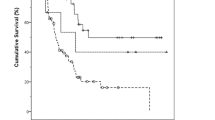
Intestinal-type ampullary adenocarcinomas had similar frequency of poor histopathologic factors compared to duodenal adenocarcinomas, and pancreatobiliary-type ampullary adenocarcinomas had similar frequency of poor histopathologic factors compared to pancreatobiliary-type biliary and pancreatic adenocarcinomas. Adjusting for tumor size and nodal involvement, there was no difference in long-term survival between patients with intestinal-type ampullary, duodenal, or biliary and pancreatic tumors (p = 0.79), and there was no difference in long-term survival between patients with pancreatobiliary-type ampullary, biliary, or pancreatic tumors (p = 0.41).
Conclusions
Long-term survival for patients with ampullary carcinomas equals pancreatic, biliary, and duodenal carcinomas when the same histologic type is compared. It can be questioned whether ampullary carcinomas should be regarded as a separate entity in classification of solid tumors. Clinical trials on adjuvant treatments for periampullary carcinomas should stratify by pancreatobiliary type versus intestinal type of histologic differentiation.




Similar content being viewed by others
References
Sarmiento JM, Nagomey DM, Sarr MG, Farnell MB. Periampullary cancers: are there differences? Surg Clin North Am. 2001;81:543–55.
Riall TS, Cameron JL, Lillemoe KD, et al. Resected periampullary adenocarcinoma: 5-year survivors and their 6- to 10-year follow-up. Surgery. 2006;140:764–72.
Albores-Saavedra J, Schwartz AM, Batich K, Henson DE. Cancers of the ampulla of Vater: demographics, morphology, and survival based on 5,625 cases from the SEER program. J Surg Oncol. 2009;100:598–605.
Winter JM, Cameron JL, Olino K, et al. Clinicopathologic analysis of ampullary neoplasms in 450 patients: implications for surgical strategy and long-term prognosis. J Gastrointest Surg. 2010;14:379–87.
Albores-Saavedra J, Henson DE, Klimstra DS. Malignant epithelial tumors of the ampulla. In: Tumors of the gallbladder, extrahepatic bile ducts, and ampulla of Vater. Washington, DC: Armed Forces Institute of Pathology; 2000. p. 259–316.
Albores-Saavedra J, Hruban RH, Klimstra DS, Zamboni G. Invasive adenocarcinoma of the ampullary region. In: Bosman FT, Carneiro F, Hruban RH, Theise ND, editors. WHO classification of tumours of the digestive system. Lyon: IARC; 2010. p. 87–91.
Heinrich S, Clavien PA. Ampullary cancer. Curr Opin Gastroenterol. 2010;26:280–5.
Westgaard A, Tafjord S, Farstad IN, et al. Pancreatobiliary versus intestinal histologic type of differentiation is an independent prognostic factor in resected periampullary adenocarcinoma. BMC Cancer. 2008;8:170.
Schirmacher P, Buchler MW. Ampullary adenocarcinoma—differentiation matters. BMC Cancer. 2008;8:251.
Carter JT, Grenert JP, Rubenstein L, Stewart L, Way LW. Tumors of the ampulla of Vater: histopathologic classification and predictors of survival. J Am Coll Surg. 2008;207:210–8.
Bosnan FT. WHO classification of tumours of the digestive system. Lyon: IARC; 2010.
Verbeke CS, Gladhaug IP. Resection margin involvement and tumour origin in pancreatic head cancer. Br J Surg. 2012;99:1036–49.
Carpelan-Holmstrom M, Nordling S, Pukkala E, et al. Does anyone survive pancreatic ductal adenocarcinoma? A nationwide study re-evaluating the data of the Finnish Cancer Registry. Gut. 2005;54:385–7.
Westgaard A, Laronningen S, Mellem C, et al. Are survival predictions reliable? Hospital volume versus standardisation of histopathologic reporting for accuracy of survival estimates after pancreatoduodenectomy for adenocarcinoma. Eur J Cancer. 2009;45:2850–9.
Westgaard A, Clausen OPF, Gladhaug IP. Survival estimates after pancreatoduodenectomy skewed by non-standardized histopathology reports. APMIS. 2011;119:689–700.
Westgaard A, Schjolberg AR, Cvancarova M, Eide TJ, Clausen OPF, Gladhaug IP. Differentiation markers in pancreatic head adenocarcinomas: MUC1 and MUC4 expression indicates poor prognosis in pancreatobiliary differentiated tumours. Histopathology. 2009;54:337–47.
Kim WS, Choi DW, Choi SH, Heo JS, You DD, Lee HG. Clinical significance of pathologic subtype in curatively resected ampulla of Vater cancer. J Surg Oncol. 2012;105:266–72.
Romiti A, Barucca V, Zullo A, et al. Tumors of ampulla of Vater: a case series and review of chemotherapy options. World J Gastrointest Oncol. 2012;4:60–7.
Amptoulach S, Josefsson A, Kavantzas N, Kalaitzakis E. Adenocarcinoma of the ampulla of Vater: does the histopathologic type matter? Scand J Gastroenterol. 2011;46:1401–3.
Kimura W, Futakawa N, Yamagata S, et al. Different clinicopathologic findings in two histologic types of carcinoma of papilla of Vater. Jpn J Cancer Res. 1994;85:161–6.
Ampulla of Vater. In: Edge SB, Byrd DR, Compton CC, Fritz AG, Green FL, Trotti A, editors. AJCC cancer staging manual. 7th edition. Chicago: Springer; 2010. p. 235–40.
Frierson HF Jr. The gross anatomy and histology of the gallbladder, extrahepatic bile ducts, Vaterian system, and minor papilla. Am J Surg Pathol. 1989;13:146–62.
Verbeke CS. Resection margins and R1 rates in pancreatic cancer—are we there yet? Histopathology. 2008;52:787–96.
Kohler I, Jacob D, Budzies J, et al. Phenotypic and genotypic characterization of carcinomas of the papilla of Vater has prognostic and putative therapeutic implications. Am J Clin Pathol. 2011;135:202–11.
Albores-Saavedra J, Simpson K, Dancer YJ, Hruban R. Intestinal type adenocarcinoma: a previously unrecognized histologic variant of ductal carcinoma of the pancreas. Ann Diagn Pathol. 2007;11:3–9.
Pour PM, Pandey KK, Batra SK. What is the origin of pancreatic adenocarcinoma? Mol Cancer. 2003;2:13.
Albores-Saavedra J, Henson DE, Klimstra DS. Dysplasia, carcinoma in situ, and invasive carcinoma of the extrahepatic bile ducts. In: Tumors of the gallbladder, extrahepatic bile ducts, and ampulla of Vater. Washington, D.C.: Armed Forces Institute of Pathology; 2000. p. 191–215.
de Jong MC, Tsai S, Cameron JL, et al. Safety and efficacy of curative intent surgery for peri-ampullary liver metastasis. J Surg Oncol. 2010;102:256–63.
Kurosaki I, Minagawa M, Kitami C, Takano K, Hatakeyama K. Hepatic resection for liver metastases from carcinomas of the distal bile duct and of the papilla of Vater. Langenbecks Arch Surg. 2011;396:607–13.
National Comprehensive Cancer Network. NCCN Clinical practice guidelines in oncology. Pancreatic adenocarcinoma. Version 1.2012. http://www.nccn.org/professionals/physician_gls/pdf/pancreatic.pdf.
Furuse J, Takada T, Miyazaki M, et al. Guidelines for chemotherapy of biliary tract and ampullary carcinomas. J Hepatobiliary Pancreat Surg. 2008;15:55–62.
Struck A, Howard T, Chiorean EG, Clarke JM, Riffenburgh R, Cardenes HR. Non-ampullary duodenal adenocarcinoma: factors important for relapse and survival. J Surg Oncol. 2009;100:144–8.
Bhatia S, Miller RC, Haddock MG, Donohue JH, Krishnan S. Adjuvant therapy for ampullary carcinomas: the Mayo Clinic experience. Int J Radiat Oncol Biol Phys. 2006;66:514–9.
Narang AK, Miller RC, Hsu CC, et al. Evaluation of adjuvant chemoradiation therapy for ampullary adenocarcinoma: the Johns Hopkins Hospital—Mayo Clinic collaborative study. Radiat Oncol. 2011;6:126.
Lazaryan A, Kalmadi S, Almhanna K, Pelley R, Kim R. Predictors of clinical outcomes of resected ampullary adenocarcinoma: a single-institution experience. Eur J Surg Oncol. 2011;37:791–7.
Neoptolemos JP, Moore MJ, Cox TF, et al. Ampullary cancer ESPAC-3 (v2) trial: A multicenter, international, open-label, randomized controlled phase III trial of adjuvant chemotherapy versus observation in patients with adenocarcinoma of the ampulla of Vater. J Clin Oncol. 2011;29(Suppl):LBA4006.
Acknowledgment
The authors gratefully acknowledge all colleagues at the Department of Pathology, Oslo University Hospital, and Svetlana Tafjord in particular, for invaluable help in prospective classification of pancreatoduodenectomy resection specimens.
Conflict of interest
None declared.
Ethical Approval
The study was approved by the Regional Committee for Medical and Health Research Ethics for Southern Norway.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Westgaard, A., Pomianowska, E., Clausen, O.P.F. et al. Intestinal-type and Pancreatobiliary-type Adenocarcinomas: How Does Ampullary Carcinoma Differ from Other Periampullary Malignancies?. Ann Surg Oncol 20, 430–439 (2013). https://doi.org/10.1245/s10434-012-2603-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-012-2603-0