Abstract
Background
18F-fluorodeoxyglucose positron emission tomography (FDG-PET) has been used extensively to explore whether FDG Uptake can be used to provide prognostic information for esophageal cancer patients. The aim of the present review is to evaluate the literature available to date concerning the potential prognostic value of FDG uptake in esophageal cancer patients, in terms of absolute pretreatment values and of decrease in FDG uptake during or after neoadjuvant therapy.
Methods
A computer-aided search of the English language literature concerning esophageal cancer and standardized uptake values was performed. This search focused on clinical studies evaluating the prognostic value of FDG uptake as an absolute value or the decrease in FDG uptake and using overall mortality and/or disease-related mortality as an end point.
Results
In total, 31 studies met the predefined criteria. Two main groups were identified based on the tested prognostic parameter: (1) FDG uptake and (2) decrease in FDG uptake. Most studies showed that pretreatment FDG uptake and postneoadjuvant treatment FDG uptake, as absolute values, are predictors for survival in univariate analysis. Moreover, early decrease in FDG uptake during neoadjuvant therapy is predictive for response and survival in most studies described. However, late decrease in FDG uptake after completion of neoadjuvant therapy was predictive for pathological response and survival in only 2 of 6 studies.
Conclusions
Measuring decrease in FDG uptake early during neoadjuvant therapy is most appealing, moreover because the observed range of values expressed as relative decrease to discriminate responding from nonresponding patients is very small. At present inter-institutional comparison of results is difficult because several different normalization factors for FDG uptake are in use. Therefore, more research focusing on standardization of protocols and inter-institutional differences should be performed, before a PET-guided algorithm can be universally advocated.
Similar content being viewed by others
Esophageal cancer is an aggressive disease with early dissemination. Even after potentially curative surgery, long-term survival rates rarely exceed 35%.1,2 In order to improve this outcome, institutes apply neoadjuvant chemotherapy and/or radiotherapy; however, only patients who respond to this therapy benefit.3–7
Assessment of prognosis can influence patient management; a diagnostic test that provides pretreatment prognostic information will therefore have additional value. Moreover, prediction of tumor response early, during the neoadjuvant regimen, is of crucial importance. 18F-fluorodeoxyglucose positron emission tomography (FDG-PET) is a noninvasive imaging technique that enables quantification of tumor activity on the basis of altered tissue glucose metabolism.8–10 Many studies have been published on the improvement of preoperative staging of esophageal cancer with FDG-PET by detecting distant metastases.11–13 FDG-PET also seems to be a valuable tool to monitor early response to neoadjuvant therapy.14–16 Evidence for reliable and useful response measurement in esophageal cancer patients is growing, while response measurement is already well established in, for example, non-small cell lung cancer and lymphoma.17–21
Recent literature suggests that FDG-PET at time of diagnosis might be useful for prognostication. The underlying idea is that the quantity of FDG activity in the tumor correlates with viable tumor cell number and thus with prognosis.22–26 The most commonly applied (semi-) quantification parameter in clinical PET is the standardized uptake value (SUV) of the primary tumor. SUV is determined by the ratio of activity in the region of interest (Bq/mL) over the decay-corrected activity of FDG injected into the patient (Bq/g).27,28
The present review evaluates the literature available to date concerning the potential prognostic value of FDG uptake in esophageal cancer patients, in terms of absolute pretreatment value and of decrease in FDG uptake during or after neoadjuvant therapy.
Literature Search
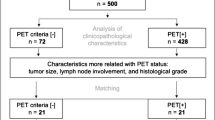
A review of the English language literature concerning esophageal cancer and standardized uptake values was performed. A computer-aided search was performed of the databases PubMed and Embase in January 2009. The terms “positron emission tomography,” “FDG-uptake,” “SUV,” and “esophageal cancer,” with restriction to the English language only, were used.29 All searches were performed using text word or medical subject heading (MeSH). Searches were focused on clinical studies evaluating the prognostic value of FDG uptake as an absolute value or the decrease in FDG uptake (during neoadjuvant therapy), possibly in combination with other factors, and using overall mortality and/or disease related mortality as an end point in esophageal cancer patients. Two researchers (J.M.T.O. and M.v.H.) read all abstracts and evaluated whether an abstract met the predefined criteria. After this selection, all publications were retrieved as full papers and re-evaluated for inclusion.
Results
In total, 31 studies met the predefined criteria.14,16,30–59 Two main groups were identified based on the tested prognostic parameter: (1) FDG uptake and (2) decrease in FDG uptake. In the first group, 15 studies described FDG uptake measured before any form of treatment was started (group 1A: Table 1), and 5 studies described FDG uptake measured after neoadjuvant treatment (group 1B: Table 2).30–44,52–56 In the second group, 6 studies described decrease in FDG uptake measured early during neoadjuvant therapy (group 2A: Table 3), and also 10 studies described decrease in FDG uptake measured after completion of neoadjuvant therapy (group 2B: Table 3).14,16,38,41,42,45–51,55,57–59 Also, 9 studies described the same cohorts of patients; however these were not excluded.31,32,35,36,41,42,47,49,51 Methodological aspects of included studies are described in Tables 4, 5, and 6.
FDG Uptake as Prognostic Factor (Group 1)
Group 1A: Pretreatment FDG Uptake and Prognosis (Table 1)
In 1998 Fukunaga et al. found in 48 patients that even though clinicopathological findings did not correlate with FDG uptake, patients with a high SUV had a poorer prognosis compared with those with low FDG uptake (55% 2-year disease-free survival vs 30%).33 This study is limited by the lack of multivariate analysis. In 2002 Kato et al. showed that FDG uptake was associated with depth of tumor invasion, presence of lymph node metastases, and lymphatic vessel invasion in 32 patients.35 The 2-year survival rate in patients with high FDG uptake (48%) was lower than in patients with low FDG uptake (91%). It would have been helpful if the authors had provided 95% confidence intervals for these survival rates. In another publication on partly the same cohort, a significant correlation was found between FDG uptake and Glut-1 expression; low Glut-1 expression and low FDG uptake appeared to carry a better prognosis: these patients showed 100% 2-year survival (n = 15).36 Multivariate analysis was unfortunately not performed.
Choi et al. showed in a multivariate analysis that only PET + lnn was an independent prognostic factor for disease-free survival.31 In multivariate analysis for overall survival only cTNM, pTNM, PET tumor length, and PET + lnn were independent predictive factors. The large proportion of patients with squamous cell carcinomas included in this study limits the use of these results in western populations. In another publication on partly the same cohort multivariate analysis showed pTNM, PET + lnn, VEGF expression, and intratumoral microvessel density (MVD) to be independent predictors for overall survival. A total of 7 variables were included in the multivariate regression model, well exceeding the generally acceptable number of 1 variable per every 10 events and thus increasing the risk of coincidental findings.32
Hong et al. showed in 47 patients with locoregional esophageal cancer that the number of PET abnormalities (NPA) correlates with overall and disease-free survival in univariate and multivariate analysis, while FDG uptake did not.34 Only half of the patients underwent esophagectomy (no explanation provided). Clinical TNM stage was not included in this analysis to assess independent value of NPA. Stahl et al. showed in a retrospectively analyzed cohort of 40 patients with esophageal cancer that FDG uptake in the primary tumor did not correlate with overall survival.40 The authors suggest that the reason for this might be because they only included adenocarcinomas.
Van Westreenen et al. investigated the relation between FDG uptake and the stage of disease and whether FDG uptake could be used to predict resectability and survival in 40 retrospectively collected patients with any stage of disease.43 Patients with high FDG uptake had a worse mean survival rate compared with patients with low FDG uptake (9 months compared with 20 months; P = .02). Patients eligible for resection showed a significantly lower FDG uptake compared with those with irresectable disease.
Cerfolio and Bryant showed in a multivariate analysis that patients with high FDG uptake were more likely to have poorly differentiated tumors and advanced stage using a retrospective cohort of 89 patients.30 Remarkably, FDG uptake correlated better with survival than pathological TNM stage. The 4-year survival of patients with low FDG uptake was 89% and only 31% in patients with high FDG uptake. It was, however, stated that many different pathologists with unspecified experience were used for staging the resection specimens.
Rizk et al. found that 3-year survival was 95% for patients with low FDG uptake and 57% for patients with high FDG uptake, in a retrospective analysis of 50 patients with resectable adenocarcinoma of the distal esophagus.39 The survival advantage for patients with low FDG uptake was even seen in a subset of patients with clinically and pathologically early-stage disease. This finding is quite remarkable considering the range of survival in this group of patients compared with a group of patients with all stages of disease.
Westerterp et al. investigated biological parameters to predict in which patients FDG-PET could be of prognostic value, in 26 patients.44 No association was found between FDG uptake and angiogenic markers, hexokinase isoforms, Ki-67 antigen expression, cleaved caspase-3, cell density, differentiation grade, CD68, mucus, or necrosis. Glut-1 expression showed a significant correlation with FDG uptake. They concluded that Glut-1 may be used to select esophageal cancer patients in whom FDG-PET is of diagnostic value. Even in the subgroup of patients who underwent a microscopically radical resection a strong association was found between SUV and survival (P = .001).
In one of the largest available prospective studies, Omloo et al. assessed the prognostic importance of SUV and EUS parameters.56 In 125 patients who underwent esophagectomy without neoadjuvant therapy SUV, tumor location, EUS T-stage, EUS N-stage, and clinical stage proved to be of prognostic significance in univariate analysis. In multivariate analysis, however, EUS T-stage appeared to be the only independent predictor for survival.
Cheze-Le Rest et al. investigates a total of 52 patients with all stages of disease; performance of potentially curative surgery, SUVmax >9 and 2 or more PET abnormalities were significant prognostic predictors.53 In multivariate analysis, only SUVmax >9 and the presence of FDG-positive lymph nodes were found as independent predictors of poor outcome. Notably, 2 of 3 PET-derived parameters were almost identical: presence of >1 FDG-PET positive node and presence of >2 FDG-PET positive nodes. In the largest available study Chatterton et al. aimed to determine the impact of PET on clinical management and prognosis in 129 potentially curable patients.52 Significant changes in management were observed in 38% of patients, primarily as a result of the identification of additional sites.
Makino et al. found SUVmax <12 and the number of positive lymph nodes (PET + LNN) on PET before therapy to be of prognostic significance in a retrospective cohort of 38 patients with positive lymph nodes scheduled to undergo neoadjuvant chemotherapy.55 Unfortunately only 38 of 63 patients who met the inclusion criteria were included.
In summary, most studies (12 of 15) showed that pretreatment FDG uptake is a predictor for survival in univariate analysis, whereas only 2 studies showed FDG uptake to be a predictor of survival in multivariate analysis.30–33,35,36,39,43,44,53,55,56 More importantly, neither of the 2 largest prospective trials could prove the prognostic significance of FDG-PET.52,56
Group 1B: Residual Postneoadjuvant Treatment FDG Uptake and Prognosis (Table 2)
In a prospective trial, Swisher et al. reported postneoadjuvant treatment FDG-PET uptake to be able to predict response, but failed to accurately rule out microscopic residual tumor (R1 resection) in 18% of a total of 83 patients.41 Swisher et al. evaluated a similar cohort of patients to assess the utility of PET, endoscopic ultrasonography (EUS), and CT to predict pathologic response and survival.42 FDG uptake was most accurate to predict long-term survival after neoadjuvant therapy. As before, they concluded that FDG uptake cannot rule out residual disease and that esophagectomy should remain part of the therapy. Because many of the patients in this study also seem included in the previously described study by Swisher et al., these reports should not be regarded as 2 separate studies.41
Konski et al. found a correlation between the depth of tumor invasion (determined by endoscopic ultrasonography) and the baseline FDG uptake in 81 patients undergoing definitive or preoperative chemoradiotherapy.37 Only posttreatment FDG uptake predicted disease-free survival in the definitive chemoradiotherapy group. The authors state to be cautious when using posttreatment FDG uptake to determine the necessity of surgical resection, as in this group of patients no correlation between FDG uptake and disease-free survival was found. It remains unclear which variables were used in multivariate analysis, complicating data interpretation.
In a relatively small study Mamede et al. showed that FDG uptake measured before treatment correlated with clinical T stage, advanced clinical stage, tumor length, and tumor volume as determined on PET.38 FDG uptake measured after treatment was the best predictor of disease progression. The authors conclude that FDG uptake should have a definite role in the evaluation of response to therapy and in the prediction of progression-free survival, which seems rather progressive considering the number of included patients (n = 25).
Higuchi et al. showed low FDG uptake after neoadjuvant treatment to be predictive for long-term survival (P = .0071); SUV was measured in 29 of 50 patients who were included.54 Unfortunately, multivariate analysis including histopathological response was not performed.
In summary, all 5 studies showed that FDG uptake after neoadjuvant therapy was predictive for survival in univariate analysis; however, in multivariate analysis only 1 study showed FDG uptake to be independently predictive for survival.37,38,41,42,54
Decrease in FDG Uptake as Prognostic Factor (Group 2)
Group 2A: Decrease in FDG Uptake Early During Neoadjuvant Treatment and Prognosis (Table 3)
In 2001 Weber et al. evaluated in a small but well-performed study whether reduction of FDG uptake can predict response 14 days after start of neoadjuvant chemotherapy.49 A significant difference in reduction of FDG uptake was found between responding (−54%) and nonresponding patients (−15%). Applying the optimal ROC-derived cutoff value of 35% reduction as criterion for metabolic response, FDG-PET predicted histopathological response with a sensitivity of 93% (14 of 15 patients) and a specificity of 95% (21 of 22). Patients without metabolic response were characterized by significantly shorter 2-year overall survival (37% vs 60%, P = .04).
This same group of investigators validated the previous findings using this definition of metabolic response, using 65 patients.47 Metabolically responding patients showed a high histopathologic response rate (44%) with a 3-year survival rate of 70%. Metabolically nonresponding patients showed a histopathologic response rate of only 5%, and a 3-year survival rate of 35% (P = .01). The authors concluded that this study provides the basis for clinical trials in which preoperative treatment is discontinued for patients without metabolic response early in the course of therapy.
To assess the feasibility of a PET-response-guided treatment algorithm, the same group of investigators conducted a prospective single-center study, including 119 patients all of whom underwent 2 weeks of neoadjuvant chemotherapy and subsequent evaluation.14 After 2 weeks, metabolic responders (FDG uptake decrease >35%) continued to receive neoadjuvant chemotherapy for 12 more weeks; nonresponders discontinued neoadjuvant treatment and proceeded to immediate surgery. In addition, 58% of the metabolic responders also appeared to be histopathological responders. Median disease-free survival in metabolic responders was 30 months compared with 14 months in metabolic nonresponders. These results could at least partly be explained by the fact that metabolic responders underwent a total of 14 weeks of chemotherapy, whereas nonresponders only had 2 weeks of chemotherapy.
In another study from this same group of investigators, FDG-PET was performed before initiation of chemotherapy, 14 days after the start and preoperatively in 24 patients.51 Changes in FDG uptake at both time points were significantly correlated with histopathologic response, and reduction in FDG uptake early in the course of therapy was also significantly correlated with survival (P = .03).
In 2004 Wieder et al. analyzed 38 patients with squamous cell carcinomas treated with neoadjuvant chemoradiotherapy and subsequent esophagectomy.50 Histopathological responders showed a decrease of 44% in FDG uptake after 2 weeks of therapy, compared with 21% in histopathological nonresponders (P = .06). Metabolic changes were significantly correlated with survival (P = .01).
In 2006 Westerterp et al. performed FDG-PET before start and after 14 days of neoadjuvant thermochemoradiotherapy.16 In histopathological responders the median decrease in FDG uptake was 44%, compared with 15% in nonresponders. At a cutoff value of 31% decrease in FDG uptake compared with baseline, sensitivity to detect response was 75% with a corresponding specificity of also 75%.
In summary, all 6 of the aforementioned studies showed that early decrease in FDG uptake is predictive for pathological response. All but 1 study showed decrease in FDG uptake also to be predictive for survival.16 Unfortunately, 5 of 6 of these studies were performed in 1 single institute, underlining the need for new multicenter studies to confirm these findings.
Group 2B: Decrease in FDG Uptake Postneoadjuvant Treatment and Prognosis (Table 3)
Port et al. retrospectively reviewed the ability of FDG-PET to predict clinical and pathological response to preoperative chemotherapy in 62 patients.48 Almost 60% of the patients showed ≥ 50% decrease in FDG uptake, showing a better survival compared with metabolically nonresponding patients (36 vs 18 months, P = .03). Multivariate analysis showed metabolic response to be the only significant predictor for disease-free survival. Including 5 variables in a multivariate model with roughly 60 patients and 30 events is, however, a stretch.
Makino et al. found that patients with a decrease in SUV above the cutoff value of 70% showed significantly better survival.55 Decrease in uptake in the primary tumor as well as in lymph nodes were associated with survival.
In 2003 Downey et al. found that stratification below or above 60% decrease in FDG uptake leads to a 2-year survival of 38% in metabolic nonresponders compared with 67% for metabolic responders (P = .06).45 No details were provided as to why only 39 of a total of 184 patients were included in this study.
In 2006 Levine et al. evaluated a total of 64 patients who underwent PET before the initiation of therapy and 4–6 weeks after completion of therapy.46 A decrease in absolute FDG uptake was predictive of histopathological response (P = .05), not for survival.
The study of Mamede et al. found a 32% decrease in FDG uptake to be the best cutoff value for histopathological response with 75% sensitivity and 63% specificity and for disease-free survival.38
Roedl et al. found the highest accuracy to predict response and survival using the decrease of the diameter-SUV index, a decrease of 55% or more identified pathologic responders with a sensitivity of 91% and a specificity of 93%.58 Metabolic responders had a mean disease-free survival of 32 months, nonresponders 16 months (P = .001).
In another study of Roedl et al., 51 patients with adenocarcinoma were studied.57 Decrease in tumor volume appeared to be a better predictor for response and survival compared with decrease in SUV. The highest accuracy was achieved using the total lesion glycolysis (calculated by multiplying the tumor volume using the mean SUV of the volume) to identify treatment responders.
Schmidt et al. found neither baseline nor preoperative nor SUV reduction to correlate significantly with response or survival in 55 patients treated with neoadjuvant chemoradiotherapy.59
In summary, decrease in FDG uptake after completion of neoadjuvant therapy was predictive for response and survival in only 4 of 10 studies.38,48,55,57 Remarkably, these studies included fewer patients and showed lower percentages of responding patients compared with the other 6 studies. Despite some positive findings, none of these studies suggests that these posttreatment prediction models should have any therapeutic consequences.
Discussion and Conclusion
Most studies showed that pretreatment FDG uptake and postneoadjuvant treatment FDG uptake as absolute values are predictors for survival in univariate analysis. Moreover, early decrease in FDG uptake during neoadjuvant therapy is predictive for response and survival in most studies described. However, late decrease in FDG uptake after completion of neoadjuvant therapy was predictive for response and survival in only 2 of 6 studies. A major disadvantage is that some studies included patients with a wide range of disease (adenocarcinomas and squamous cell carcinomas, stage I through IV) and studies used different neoadjuvant treatment regimens. Especially those studies that describe patients receiving radiotherapy, it is known FDG uptake in these patients remains higher compared with patients receiving only chemotherapy. Most importantly, all institutes used different scanners with different protocols and used different reconstruction methods, and these heterogeneous data made pooling of results impossible.
Many prognostic factors, determined pretreatment and/or posttreatment, for example, TNM stage, histopathology results, and PET-derived parameters (including SUV, metabolic tumor volume, and total lesion glucolysis) are used to predict survival in esophageal cancer patients.60 In clinical practice, these factors are communicated with the patient to choose the most appropriate therapy. However, before a PET-guided treatment algorithm can be reliably implemented, more research focusing on standardization of protocols and inter-institutional technical differences should be performed in larger patient cohorts.
To date, it is difficult to compare results from different institutes and more importantly, published cutoff values are method specific and often institute specific, especially since they are also affected by acquisition protocol, reconstruction algorithm, and region of interest definition.61,62 Most importantly, to overcome these problems large multicenter prospective trials are necessary.
In conclusion, FDG-PET seems to be useful for prognostication and (neo)adjuvant treatment response assessment in esophageal cancer. However, more attention has to be paid in standardization of FDG-PET acquisition and reconstruction.
References
Hulscher JB, van Sandick JW, de Boer AG, Wijnhoven BP, Tijssen JG, Fockens P, et al. Extended transthoracic resection compared with limited transhiatal resection for adenocarcinoma of the esophagus. N Engl J Med. 2002;347:1662–9.
Omloo JM, Lagarde SM, Hulscher JB, JB, Reitsma JB, Fockens P, van Dekken H, et al. Extended transthoracic resection compared with limited transhiatal resection for adenocarcinoma of the mid/distal esophagus: five-year survival of a randomized clinical trial. Ann Surg. 2007;246:992–1001.
Cunningham D, Allum WH, Stenning SP, Thompson JN, Van de Velde CJ, Nicolson M, et al. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med. 2006;355:11–20.
Gebski V, Burmeister B, Smithers BM, Foo K, Zalcberg J, Simes J. Survival benefits from neoadjuvant chemoradiotherapy or chemotherapy in oesophageal carcinoma: a meta-analysis. Lancet Oncol. 2007;8:226–34.
Kelsen DP, Winter KA, Gunderson LL, Mortimer J, Estes NC, Haller DG, et al. Long-term results of RTOG trial 8911 (USA Intergroup 113): a random assignment trial comparison of chemotherapy followed by surgery compared with surgery alone for esophageal cancer. J Clin Oncol. 2007;25:3719–25.
van Meerten E., Muller K, Tilanus HW, Siersema PD, Eijkenboom WM, van Dekken H, et al. Neoadjuvant concurrent chemoradiation with weekly paclitaxel and carboplatin for patients with oesophageal cancer: a phase II study. Br J Cancer. 2006;94:1389–94.
Ancona E, Ruol A, Santi S, Merigliano S, Sileni VC, Koussis H, et al. Only pathologic complete response to neoadjuvant chemotherapy improves significantly the long term survival of patients with resectable esophageal squamous cell carcinoma: final report of a randomized, controlled trial of preoperative chemotherapy versus surgery alone. Cancer. 2001;91:2165–74.
Czernin J, Phelps ME. Positron emission tomography scanning: current and future applications. Annu Rev Med. 2002;53:89–112.
Gambhir SS, Czernin J, Schwimmer J, J, Silverman DH, Coleman RE, Phelps ME. A tabulated summary of the FDG PET literature. J Nucl Med. 2001;42:1S–93S.
Rohren EM, Turkington TG, Coleman RE. Clinical applications of PET in oncology. Radiology. 2004;231:305–32.
Flamen P, Lerut A, Van CE, Cambier JP, Maes A, De Wever W, et al. Utility of positron emission tomography for the staging of patients with potentially operable esophageal carcinoma. J Clin Oncol. 2000;18:3202–10.
Kato H, Miyazaki T, Nakajima M, Takita J, Kimura H, Faried A, et al. The incremental effect of positron emission tomography on diagnostic accuracy in the initial staging of esophageal carcinoma. Cancer. 2005;103:148–56.
van Westreenen HL, Westerterp M, Sloof GW, Groen H, Bossuyt PM, Jager PL, et al. Limited additional value of positron emission tomography in staging oesophageal cancer. Br J Surg. 2007;94;1515–20.
Lordick F, Ott K, Krause BJ, Weber WA, Becker K, Stein HJ, et al. PET to assess early metabolic response and to guide treatment of adenocarcinoma of the oesophagogastric junction: the MUNICON phase II trial. Lancet Oncol. 2007;8:797–805.
Westerterp M, van Westreenen HL, Reitsma JB, Hoekstra OS, Stoker J, Fockens P, et al. Esophageal cancer: CT, endoscopic US, and FDG PET for assessment of response to neoadjuvant therapy—systematic review. Radiology. 2005;236:841–51.
Westerterp M, Omloo JM, Sloof GW, Hulshof MC, Hoekstra OS, Crezee H, et al. Monitoring of response to pre-operative chemoradiation in combination with hyperthermia in oesophageal cancer by FDG-PET. Int J Hyperthermia. 2006;22:149–60.
Dooms C, Verbeken E, Stroobants S, Nackaerts K, De Leyn P, Vansteenkiste J. Prognostic stratification of stage IIIA-N2 non-small-cell lung cancer after induction chemotherapy: a model based on the combination of morphometric-pathologic response in mediastinal nodes and primary tumor response on serial 18-fluoro-2-deoxy-glucose positron emission tomography. J Clin Oncol. 2008;26:1128–34.
Hoekstra CJ, Hoekstra OS, Stroobants SG, Vansteenkiste J, Nuyts J, Smit EF, et al. Methods to monitor response to chemotherapy in non-small cell lung cancer with 18F-FDG PET. J Nucl Med. 2002;43:1304–9.
Hoekstra CJ, Stroobants SG, Smit EF, Vansteenkiste J, van Tinteren H, Postmus PE, et al. Prognostic relevance of response evaluation using [18F]-2-fluoro-2-deoxy-d-glucose positron emission tomography in patients with locally advanced non-small-cell lung cancer. J Clin Oncol. 2005;23:8362–70.
Krak NC, Boellaard R, Hoekstra OS, Twisk JW, Hoekstra CJ, Lammertsma AA. Effects of ROI definition and reconstruction method on quantitative outcome and applicability in a response monitoring trial. Eur J Nucl Med Mol Imaging. 2005;32:294–301.
Juweid ME, Stroobants S, Hoekstra OS, Mottaghy FM, Dietlein M, Guermazi A, et al. Use of positron emission tomography for response assessment of lymphoma: consensus of the Imaging Subcommittee of International Harmonization Project in Lymphoma. J Clin Oncol. 2007;25:571–8.
Allal AS, Slosman DO, Kebdani T, Allaoua M, Lehmann W, Dulguerov P. Prediction of outcome in head-and-neck cancer patients using the standardized uptake value of 2-[18F]fluoro-2-deoxy-d-glucose. Int J Radiat Oncol Biol Phys. 2004;59:1295–300.
Downey RJ, Akhurst T, Gonen M, Vincent A, Bains MS, Larson S, et al. Preoperative F-18 fluorodeoxyglucose-positron emission tomography maximal standardized uptake value predicts survival after lung cancer resection. J Clin Oncol. 2004;22:3255–60.
Oyama N, Akino H, Suzuki Y, Kanamaru H, Miwa Y, Tsuka H, et al. Prognostic value of 2-deoxy-2-[F-18]fluoro-d-glucose positron emission tomography imaging for patients with prostate cancer. Mol Imaging Biol. 2002;4:99–104.
Schwarzbach MH, Hinz U, Dmitrakopoulou-Strauss A, Willeke F, Cardona S, Mechtersheimer G, et al. Prognostic significance of preoperative [18-F] fluorodeoxyglucose (FDG) positron emission tomography (PET) imaging in patients with resectable soft tissue sarcomas. Ann Surg. 2005;241:286–94.
Minn H, Clavo AC, Grenman R, Wahl RL. In vitro comparison of cell proliferation kinetics and uptake of tritiated fluorodeoxyglucose and l-methionine in squamous-cell carcinoma of the head and neck. J Nucl Med. 1995;36:252–8.
Boellaard R, Krak NC, Hoekstra OS, Lammertsma AA. Effects of noise, image resolution, and ROI definition on the accuracy of standard uptake values: a simulation study. J Nucl Med. 2004;45:1519–27.
Thie JA. Understanding the standardized uptake value, its methods, and implications for usage. J Nucl Med. 2004;45:1431–4.
Mijnhout GS, Hooft L, van Tulder MW, Devillé WL, Teule GJ, Hoekstra OS. How to perform a comprehensive search for FDG-PET literature. Eur J Nucl Med. 2000;27:91–7.
Cerfolio RJ, Bryant AS. Maximum standardized uptake values on positron emission tomography of esophageal cancer predicts stage, tumor biology, and survival. Ann Thorac Surg. 2006;82:391–4.
Choi JY, Jang HJ, Shim YM, Kim K, Lee KS, Lee KH, et al. 18F-FDG PET in patients with esophageal squamous cell carcinoma undergoing curative surgery: prognostic implications. J Nucl Med. 2004;45:1843–50.
Choi JY, Jang KT, Shim YM, Kim K, Ahn G, Lee KH, et al. Prognostic significance of vascular endothelial growth factor expression and microvessel density in esophageal squamous cell carcinoma: comparison with positron emission tomography. Ann Surg Oncol. 2006;13:1054–62.
Fukunaga T, Okazumi S, Koide Y, Isono K, Imazeki K. Evaluation of esophageal cancers using fluorine-18-fluorodeoxyglucose PET. J Nucl Med. 1998;39:1002–7.
Hong D, Lunagomez S, Kim EE, Lee JH, Bresalier RS, Swisher SG, et al. Value of baseline positron emission tomography for predicting overall survival in patient with nonmetastatic esophageal or gastroesophageal junction carcinoma. Cancer. 2005;104:1620–6.
Kato H, Kuwano H, Nakajima M, Miyazaki T, Yoshikawa M, Ojima H, et al. Comparison between positron emission tomography and computed tomography in the use of the assessment of esophageal carcinoma. Cancer. 2002;94:921–8.
Kato H, Takita J, Miyazaki T, Nakajima M, Fukai Y, Masuda N, et al. Correlation of 18-F-fluorodeoxyglucose (FDG) accumulation with glucose transporter (Glut-1) expression in esophageal squamous cell carcinoma. Anticancer Res. 2003;23:3263–72.
Konski AA, Cheng JD, Goldberg M, Li T, Maurer A, Yu JQ, et al. Correlation of molecular response as measured by 18-FDG positron emission tomography with outcome after chemoradiotherapy in patients with esophageal carcinoma. Int J Radiat Oncol Biol Phys. 2007;69:358–63.
Mamede M, Abreu-e-Lima, Oliva MR, Nosé V, Mamon H, Gerbaudo VH. FDG-PET/CT tumor segmentation-derived indices of metabolic activity to assess response to neoadjuvant therapy and progression-free survival in esophageal cancer: correlation with histopathology results. Am J Clin Oncol. 2007;30:377–88.
Rizk N, Downey RJ, Akhurst T, Gonen M, Bains MS, Larson S, et al. Preoperative 18[F]-fluorodeoxyglucose positron emission tomography standardized uptake values predict survival after esophageal adenocarcinoma resection. Ann Thorac Surg. 2006;81:1076–81.
Stahl A, Stollfuss J, Ott K, Wieder H, Fink U, Schwaiger M, et al. FDG PET and CT in locally advanced adenocarcinomas of the distal oesophagus. Clinical relevance of a discordant PET finding. Nuklearmedizin. 2005;44:249–55.
Swisher SG, Erasmus J, Maish M, Correa AM, Macapinlac H, Ajani JA, et al. 2-Fluoro-2-deoxy-d-glucose positron emission tomography imaging is predictive of pathologic response and survival after preoperative chemoradiation in patients with esophageal carcinoma. Cancer. 2004;101:1776–85.
Swisher SG, Maish M, Erasmus JJ, Correa AM, Ajani JA, Bresalier R, et al. Utility of PET, CT, and EUS to identify pathologic responders in esophageal cancer. Ann Thorac Surg. 2004;78:1152–60.
van Westreenen HL, Plukker JT, Cobben DC, Verhoogt CJ, Groen H, Jager PL. Prognostic value of the standardized uptake value in esophageal cancer. Am J Roentgenol. 2005;185:436–40.
Westerterp M, Sloof GW, Hoekstra OS, Ten Kate FJ, Meijer GA, Reitsma JB, et al. (18)FDG uptake in oesophageal adenocarcinoma: linking biology and outcome. J Cancer Res Clin Oncol. 2008;134:227–36.
Downey RJ, Akhurst T, Ilson D, Ginsberg R, Bains MS, Gonen M, et al. Whole body 18FDG-PET and the response of esophageal cancer to induction therapy: results of a prospective trial. J Clin Oncol. 2003;21:428–32.
Levine EA, Farmer MR, Clark P, Mishra G, Ho C, Geisinger KR, et al. Predictive value of 18-fluoro-deoxy-glucose-positron emission tomography (18F-FDG-PET) in the identification of responders to chemoradiation therapy for the treatment of locally advanced esophageal cancer. Ann Surg. 2006;243:472–8.
Ott K, Weber WA, Lordick F, Becker K, Busch R, Herrmann K, et al. Metabolic imaging predicts response, survival, and recurrence in adenocarcinomas of the esophagogastric junction. J Clin Oncol. 2006;24:4692–8.
Port JL, Lee PC, Korst RJ, Liss Y, Meherally D, Christos P, et al. Positron emission tomographic scanning predicts survival after induction chemotherapy for esophageal carcinoma. Ann Thorac Surg. 2007;84:393–400.
Weber WA, Ott K, Becker K, Dittler HJ, Helmberger H, Avril NE, et al. Prediction of response to preoperative chemotherapy in adenocarcinomas of the esophagogastric junction by metabolic imaging. J Clin Oncol. 2001;19:3058–65.
Wieder HA, Brucher BL, Zimmermann F, Becker K, Lordick F, Beer A, et al. Time course of tumor metabolic activity during chemoradiotherapy of esophageal squamous cell carcinoma and response to treatment. J Clin Oncol. 2004;22:900–8.
Wieder HA, Ott K, Lordick F, Becker K, Stahl A, Herrmann K, et al. Prediction of tumor response by FDG-PET: comparison of the accuracy of single and sequential studies in patients with adenocarcinomas of the esophagogastric junction. Eur J Nucl Med Mol Imaging. 2007;34:1925–32.
Chatterton BE, Ho S, I, Baldey A, Baldey A, Lenzo N, Patrikeos A, et al. Positron emission tomography changes management and prognostic stratification in patients with oesophageal cancer: results of a multicentre prospective study. Eur J Nucl Med Mol Imaging. 2009;36:354–61.
Cheze-Le Rest C., Metges JP, Teyton P, Jestin-Le Tallec V, Lozac’h P, Volant A, et al. Prognostic value of initial fluorodeoxyglucose-PET in esophageal cancer: a prospective study. Nucl Med Commun. 2008;29:628–35.
Higuchi I, Yasuda T, Yano M, Doki Y, Miyata H, Tatsumi M, et al. Lack of fludeoxyglucose F 18 uptake in posttreatment positron emission tomography as a significant predictor of survival after subsequent surgery in multimodality treatment for patients with locally advanced esophageal squamous cell carcinoma. J Thorac Cardiovasc Surg. 2008;136:205–12.
Makino T, Doki Y, Miyata H, Yasuda T, Yamasaki M, Fujiwara Y, et al. Use of (18)F-fluorodeoxyglucose-positron emission tomography to evaluate responses to neo-adjuvant chemotherapy for primary tumor and lymph node metastasis in esophageal squamous cell carcinoma. Surgery. 2008;144:793–802.
Omloo JM, Sloof GW, Boellaard R, Hoekstra OS, Jager PL, van Dullemen HM, et al. Importance of fluorodeoxyglucose-positron emission tomography (FDG-PET) and endoscopic ultrasonography parameters in predicting survival following surgery for esophageal cancer. Endoscopy. 2008;40:464–71.
Roedl JB, Colen RR, Holalkere NS, Fischman AJ, Choi NC, Blake MA. Adenocarcinomas of the esophagus: response to chemoradiotherapy is associated with decrease of metabolic tumor volume as measured on PET-CT. Comparison to histopathologic and clinical response evaluation. Radiother Oncol. 2008;89:278–86.
Roedl JB, Halpern EF, Colen RR, Sahani DV, Fischman AJ, Blake MA. Metabolic tumor width parameters as determined on PET/CT predict disease-free survival and treatment response in squamous cell carcinoma of the esophagus. Mol Imaging Biol. 2009;11:54–60.
Schmidt M, Bollschweiler E, Dietlein M, Mönig SP, Kobe C, Vallböhmer D, et al. Mean and maximum standardized uptake values in [18F]FDG-PET for assessment of histopathological response in oesophageal squamous cell carcinoma or adenocarcinoma after radiochemotherapy. Eur J Nucl Med Mol Imaging. 2009;36:735–44.
Hyun SH, Choi JY, Shim YM, Kim K, Lee SJ, Cho YS, et al. Prognostic value of metabolic tumor volume measured by 18F-fluorodeoxyglucose positron emission tomography in patients with esophageal carcinoma. Ann Surg Oncol. 2010;17:115–22.
Westerterp M, Pruim J, Oyen W, Hoekstra O, Paans A, Visser E, et al. Quantification of FDG PET studies using standardised uptake values in multi-centre trials: effects of image reconstruction, resolution and ROI definition parameters. Eur J Nucl Med Mol Imaging. 2007;34:392–404.
Lammertsma AA, Hoekstra CJ, Giaccone G, Hoekstra OS. How should we analyse FDG PET studies for monitoring tumour response? Eur J Nucl Med Mol Imaging. 2006;33 Suppl 1:16–21.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Additional information
J.M.T. Omloo and M. van Heijl contributed equally to this work.
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Omloo, J.M.T., van Heijl, M., Hoekstra, O.S. et al. FDG-PET Parameters as Prognostic Factor in Esophageal Cancer Patients: A Review. Ann Surg Oncol 18, 3338–3352 (2011). https://doi.org/10.1245/s10434-011-1732-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-011-1732-1