Abstract
Background
The presence of extrahepatic disease (EHD) is considered a contraindication to hepatectomy in patients with colorectal liver metastases. After resection, the prognosis is based more on the total number of resected metastases (located inside and outside the liver) than on the site of these metastases (only inside the liver or not).
Methods
A total of 308 patients with colorectal cancer underwent hepatectomy, and 84 (27%) also underwent resection of miscellaneous EHD. The study was a prospective data registration and retrospective analysis. When considering the total number of resected metastases, each liver metastasis and each EHD location was counted as one lesion. Univariate and multivariate analyses were performed.
Results
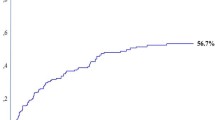
The median follow-up was 99 months. The overall 5-year survival rate was 32%. In the multivariate analysis, the total number of metastases (inside or outside the liver) had a greater prognostic value than the criterion “presence or absence of EHD.” Considering the total number of resected metastases (whatever their site), 5-year survival rates were 38% (SD: 4%) in the group with one to three metastases, 29% (SD: 5%) in patients with four to six metastases, and 18% (SD: 5%) in patients with more than six metastases (P = .002). A very simple prognostic score based on sex and the total number of metastases is proposed.
Conclusions
EHD, when resectable, is no longer a contraindication to hepatectomy. More importantly, the total number of the metastases, whatever their location, has a stronger prognostic effect than the site of these metastases.




Similar content being viewed by others
References
Hughes KS, Simon R, Songhorabodi S, et al. Resection of the liver for colorectal carcinoma metastases: a multi-institutional study of indications for resection. Surgery 1988;103:278–88
Nordlinger B, Jaeck D, Guignet M, et al. Résection Chirurgicale des Métastases Hépatiques, Enquête de l’Association Française de Chirurgie. Paris: Springer-Verlag, 1992:141–75
Eckberg H, Transberg KG, Andersson R, et al. Determinants of survival in liver resection for colorectal secondaries. Br J Surg 1986;73:727–31
Cady B, McDermott WV Jr. Major hepatic resection for metachronous metastases from colon cancer. Ann Surg 1985;210:204–9
Foster JH. Survival after liver resection for secondary tumors. Am J Surg 1978;135:389–94
Adson MA. The resection of hepatic metastases. Another view. Arch Surg 1989;124:1023–4
Fong Y, Fortner J, Sun RL, Brennan MF, Blumgart LH. Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer. Analysis of 1001 consecutive cases. Ann Surg 1999;230:309–21
Jamison RL, Donohue JH, Nagorney DM, Rosen CB, Harmsen S, Ilstrup DM. Hepatic resection for metastatic colorectal cancer results in cure for some patients. Arch Surg 1997;132:505–11
Scheele J, Stang R, Altendorf-Hofmann A, Paul M. Resection of colorectal metastases. World J Surg 1995;19:59–71
Iwatsuki S, Dvorchick I, Madariaga J, et al. Hepatic resection for metastatic colorectal adenocarcinoma: a proposal of a prognostic scoring system. J Am Coll Surg 1999;189:291–9
Chu DZ, Lang NP, Thompson C, Osteen PK, Westbrook KC. Peritoneal carcinomatosis in non-gynecologic malignancy. Cancer 1989;63:364–7
Sadeghi B, Arvieux C, Glehen O, et al. Peritoneal carcinomatosis from non-gynecologic malignancies. Multicentric prospective study. Cancer 2000;88:358–63
Minagawa M, Makuuchi M, Torzilli G, et al. Extension of the frontiers of surgical indications in the treatment of liver metastases from colorectal cancer. Ann Surg 2000;231:487–99
Imamura H, Seyama Y, Kokudo N, et al. Single and multiple resections of multiple hepatic metastases of colorectal origin. Surgery 2004;135:508–17
Ike H, Shimada H, Ohki S, Togo S, Yamaguchi S, Ichikawa Y. Results of aggressive resection of lung metastases from colorectal carcinoma detected by intensive follow-up. Dis Colon Rectum 2002;45:468–75
Regnard JF, Grunenwald D, Spaggiari L, et al. Surgical treatment of hepatic and pulmonary metastases from colorectal cancers. Ann Thorac Surg 1998;66:214–9
Elias D, Ouellet JF, Bellon N, Pignon JP, Pocard M, Lasser P. Extrahepatic disease does not contraindicate hepatectomy for colorectal liver metastases. Br J Surg 2003;90:567–74
Adam R, Pascal G, Castaing D, et al. Tumor progression while on chemotherapy. A contraindication to liver resection for multiple colorectal metastases? Ann Surg 2004;240:1052–64
Elias D, Sideris L, Pocard M, et al. Results of R0 resection for colorectal metastases associated with extrahepatic disease. Ann Surg Oncol 2004;11:274–80
Sugarbaker PH, Jablonski KH. Prognostic features of 51 colorectal and 130 appendiceal cancer patients with peritoneal carcinomatosis treated by cytoreductive surgery and intraperitoneal chemotherapy. Ann Surg 1995;221:124–32
Verwaal VC, van Ruth S, de Bree E, et al. Randomized trial of cytoreduction and hyperthermic intraperitoneal chemotherapy versus systemic chemotherapy and palliative surgery in patients with peritoneal carcinomatosis from colorectal cancer. J Clin Oncol 2003;21:3737–43
Elias D, Sideris L, Pocard M, et al. Efficacy of intraperitoneal chemohyperthermia with oxaliplatin in colorectal peritoneal carcinomatosis. Preliminary results in 24 patients. Ann Oncol 2004;15:781–5
Elias D, Ouellet JF. Intraperitoneal chemohyperthermia: rationale, technique, indications, and results. Surg Oncol Clin North Am 2001;10:915–33
Filder IJ. Seed and soil revisited. Contribution of the organ microenvironment to cancer metastases. Surg Oncol Clin North Am 2001;10:257–69
Imamura H, Shimada R, Kubota M, et al. Preoperative portal vein embolization: an audit of 84 patients. Hepatology 1999;29:1099–105
Roche A, Soyer P, Elias D, Breittmayer F, Gad M, Rougier PH. Pre-operative portal vein embolisation for hepatic metastases. J Intervent Radiol 1991;6:63–6
Elias D, Desruennes E, Lasser PH. Prolonged intermittent clamping of the portal triad during hepatectomy. Br J Surg 1991;78:42–4
Elias D, Lasser P, Debaene B, et al. Intermittent exclusion of the liver without vena cava clamping during major hepatectomy. Br J Surg 1995;82:1535–9
Elias D, Delperro JR, Sideris L, et al. Treatment of peritoneal carcinomatosis from colorectal cancer: impact of complete cytoreductive surgery and difficulties in conducting randomised trials. Ann Surg Oncol 2004;11:518–21
Elias D, Dube P, Bonvalot S, et al. Treatment of liver metastases with moderate peritoneal carcinomatosis by hepatectomy and cytoreductive surgery followed by immediate postoperative intraperitoneal chemotherapy. Feasibility and preliminary results. Hepatogastroenterology 1999;46:360–3
Elias D, Bonnay M, Puizillou JM, et al. Heated intra-operative intraperitoneal oxaliplatin after complete resection of peritoneal carcinomatosis: pharmacokinetics and tissue distribution. Ann Oncol 2002;13:267–72
Elias D, El Otmany A, Bonnay M, et al. Human pharmacokinetic study of heated intraperitoneal oxaliplatin in increasingly hypotonic solutions after complete resection of peritoneal carcinomatosis. Oncology 2002;63:346–52
Elias D, Matsuhisa T, Sideris L, et al. Heated intra-operative intraperitoneal oxaliplatin plus irinotecan after complete resection of peritoneal carcinomatosis: pharmacokinetics, tissue distribution and tolerance. Ann Oncol 2004;15:1558–65
Glehen O, Kwiatkowski F, Sugarbaker PH, et al. Cytoreductive surgery combined with intraperitoneal chemotherapy for management of peritoneal carcinomatosis from colorectal cancer: a multi-institutional study. J Clin Oncol 2004;22:3284–92
Elias D. Peritoneal carcinomatosis or liver metastases from colorectal cancer: similar standards for a curative surgery? Ann Surg Oncol 2004;11:122–3
Tsavellas G, Patel H, Aleen-Mersh TG. Detection and clinical significance of occult tumour cells in colorectal cancer. Review. Br J Surg 2001;88:1307–20
Sadahiro S, Suzuki T, Tokunaga N, et al. Detection of tumor cells in the portal and peripheral blood of patients with colorectal carcinoma using competitive reverse transcriptase-polymerase chain reaction. Cancer 2001;92:1251–8
Pollock RE, Roth JA. Cancer-induced immunosuppression: implications for therapy? Semin Surg Oncol 1989;5:414–9
Kavanaugh DY, Carbone DP. Immunologic dysfunction in cancer. Hematol Oncol Clin North Am 1996;10:927–51
Muss HB. Chemotherapy of Gynecologic Cancer. 2nd ed. New York: Wiley-Liss, 1990
IMPACT (International Multicentre Pooled Analysis of Colon Cancer Trials). Efficacy of adjuvant fluorouracil and folinic acid in colon cancer. Lancet 1995;345:939–44
Gill S, Loprinzi CL, Sargent DJ, et al. Pooled analysis of fluorouracil-based adjuvant therapy for stage II and III colon cancer: who benefits and by how much? J Clin Oncol 2004;22:1797–806
Allen PJ, Kemeny N, Jarnagin W, et al. Importance of response to neoadjuvant chemotherapy in patients undergoing resection of synchronous colorectal liver metastases. J Gastrointest Surg 2003;7:109–17
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Elias, D., Liberale, G., Vernerey, D. et al. Hepatic and Extrahepatic Colorectal Metastases: When Resectable, Their Localization Does Not Matter, But Their Total Number Has a Prognostic Effect. Ann Surg Oncol 12, 900–909 (2005). https://doi.org/10.1245/ASO.2005.01.010
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/ASO.2005.01.010