Abstract
The ESPAC-1, ESPAC-1 plus, and early ESPAC-3(v1) results (458 randomized patients; 364 deaths) were used to estimate the effectiveness of adjuvant 5FU/FA vs resection alone for pancreatic cancer using meta-analysis. The pooled hazard ratio of 0.70 (95% CI=0.55–0.88) P=0.003, and the median survival of 23.2 (95% CI=20.1–26.5) months with 5FU/FA vs 16.8 (95% CI=14.3–19.2) months with resection alone supports the use of adjuvant 5FU/FA in pancreatic cancer.
Similar content being viewed by others
Main
The results of two recent randomized controlled trials of adjuvant treatment in pancreatic cancer (Oettle et al, 2007; Regine et al, 2008) have further raised the interest regarding optimum therapy in this disease. The CONK-001 trial showed that postoperative gemcitabine significantly delayed the development of recurrent disease compared with observation alone (Oettle et al, 2007) and subsequent analysis showed improved overall median survival (Neuhaus et al, 2008). The Radiation Therapy Oncology Group Study (RTOG) 9704 trial showed no difference in the overall survival between two chemoradiotherapy regimens, although in a subgroup analysis showed that the addition of gemcitabine (rather than 5FU) to postoperative adjuvant 5FU-based chemoradiotherapy significantly improved the survival in those patients with cancer in the head of the pancreas (Regine et al, 2008).
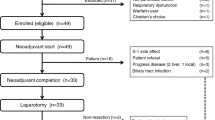
The European Study Group for Pancreatic Cancer (ESPAC) recruited 550 patients into the ESPAC-1 adjuvant trial (Figure 1) of which 289 patients were in a 2 × 2 factorial design, powered to investigate the roles of adjuvant chemotherapy (5FU with folinic acid (FA)) and chemoradiotherapy on overall survival (Neoptolemos et al, 2001, 2004). The final results confirmed that only adjuvant chemotherapy provided a significant survival benefit (Neoptolemos et al, 2004). The trial, however, was not powered for a direct comparison between the 5FU/FA and surgery alone subgroups of the 2 × 2 design. Of the 550 patients in ESPAC-1, 192 patients were entered into a direct randomised comparison between 5FU/FA and observation alone with clinician's choice of background chemoradiotherapy if indicated. This randomised comparison is referred to as the ESPAC-1 plus trial and was conducted as part of the ESPAC-1 adjuvant trial based on identical eligibility criteria and treatment schedules. Patients were recruited in parallel and in addition to the recruitment target and as such were always intended to be additional evidence not powered for analysis in isolation. The ESPAC-3(v1) trial was initially a three arm study of adjuvant 5FU/FA vs gemcitabine vs observation. Following the publication of the final results of ESPAC-1 (Neoptolemos et al, 2004), the Independent Data Monitoring Committee advised that the observation arm be dropped from ESPAC-3(v2). The Independent Data Monitoring Committee also recommended reporting of the combined results of 5FU/FA vs observation from both trials as this was planned as part of the original protocol of ESPAC-3(v1). In the 2 × 2 component of ESPAC-1 (Figure 1), patients randomised to chemotherapy (either chemotherapy alone or with chemoradiotherapy) were compared with the patients randomised not to receive chemotherapy (either surgery alone or with chemoradiotherapy) as per the 2 × 2 design, but the unexpected somewhat negative effect of chemoradiotherapy may have affected the result. Hence these data comparing the adjuvant chemotherapy alone vs surgery alone subgroups of the 2 × 2 design are important as a trial including a surgery alone arm is now unlikely to be repeated. The results are thus unique offering for the first time an unbiased randomised comparison of adjuvant 5FU/FA vs observation following the resection of pancreatic ductal adenocarcinoma. In addition, the use of meta-analysis to combine individual patient data across the three studies increases the overall sample size which, in turn, increases the statistical power of the analysis.
Methods
The inclusion criteria in ESPAC-1, ESPAC-1 plus, and ESPAC-3(v1) were identical and postoperative restaging and CA 19.9 values were not used to determine patient inclusion in these studies (Neoptolemos et al, 2001, 2004; www.cancernorth.nhs.uk/portal_repository/files/trial_sum_espac.pdf). Similarly, the chemotherapy regimen used was identical in all three studies comprising an intravenous bolus of leucovorin (folinic acid; 20 mg m−2), followed by an intravenous bolus of 5FU (425 mg m−2) on each of 5 consecutive days every 28 days for six cycles. There were 144 patients from the two groups of the ESPAC-1 2 × 2 design (69 observation, 75 5FU/FA) with a median follow-up of the 24 alive patients of 78 (interquartile range=45–92) months (Table 1). The ESPAC-1 plus component recruited 192 patients (95 observation, 19 (20%) of whom received background chemoradiotherapy; 97 5FU/FA, 25 (26%) of whom received background chemoradiotherapy) with a median follow-up of the 40 alive patients of 64 (interquartile range=20–89) months. There were 122 patients in ESPAC-3(v1) at closure of the observation arm in this trial (61 observation, 61 5FU/FA) with a median follow-up of the 30 alive patients of 54 (interquartile range=34–60) months. These data provide a direct randomised comparison of 5FU/FA vs observation alone based on the intention-to-treat principle. For the outcome of overall survival, a random effects model was used to combine the trial level hazard ratios (HRs), estimated from the individual patient data, using an inverse variance meta-analysis. Survival estimates are presented as simple, non-stratified Kaplan–Meier curves across all trials. The overall estimate of the treatment effect is adjusted by any influence of trial.
Results
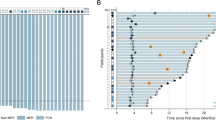
The eligibility criteria across trials were similar, and as such the patient and tumour characteristics (Table 1) were comparable with treatment schedules also identical across trials. At the time of analysis, there were 120 (83.3%) deaths in ESPAC-1, 152 (79.2%) deaths in ESPAC-1 plus, and 92 (75.4%) deaths in ESPAC-3(v1) (Table 2). The heterogeneity between trials was non-significant, and pooling the data is considered justifiable (Figures 2 and 3). The overall survival (Figure 4) was superior in patients randomized to 5FU/FA compared to those randomized to observation (pooled HR=0.70 (95% CI=0.55–0.88); P=0.003 (Table 2)) with evidence of low statistical heterogeneity (P=0.27, I2=25%, Figure 3). The pooled effect of chemotherapy is estimated to reduce the risk of death by 30% compared to surgery alone. Combined overall median survival (obtained from simple Kaplan–Meier curves non-stratified by trial) was 23.2 (95% CI=20.1–26.5) months for 5FU/FA compared to 16.8 (95% CI=14.3–19.2) months for observation with 2- and 5-year survival estimates of 49%, 24% for 5FU/FA and 37%, 14% for observation (Figures 4 and 5, Table 2). A sensitivity analysis excluding the ESPAC-1 plus study estimated that chemotherapy reduced the risk of death by 23% compared to surgery alone (HR=0.77, 95%CI=0.59, 1.01).
Discussion
This individual patient data meta-analysis of ESPAC-1, ESPAC-1 plus and ESPAC-3 trials showed significantly better overall survival for patients randomized to 5FU/FA with an HR of 0.70 (95% CI=0.55, 0.88; P=0.003) indicating a significant reduction in the risk of death of 30% with 5FU/FA compared with surgery alone.
The CONKO-001 trial (Oettle et al, 2007) found a significantly improved median disease-free survival in favour of gemcitabine (13.4 (range=11.4–15.3) months) compared to observation (6.9 (range=6.1–7.8) months; P<0.001). The overall median survival was 22.1 (range=18.4–25.8) months for the gemcitabine group, and 20.2 (range=17–23.4) months for the surgery alone group (HR=0.79 (95% CI=0.62–1.01); P=0.06). The primary end point was disease-free survival, whereas a confounding factor for overall survival was the fact that a large proportion of the control group received gemcitabine on relapse. The CONKO-001 investigators concluded that chemotherapy with gemcitabine offered the best benefit/risk ratio of all currently available adjuvant treatment options (Oettle et al, 2007). Comparison with the current study using an adjusted indirect comparison, which maintains the within trial randomisation (Bucher et al, 1997) shows that the adjuvant 5FU/FA has at least similar survival results to those of gemcitabine (adjusted indirect HR of 0.89 (95% CI=0.63–1.25) for 5FU compared with gemcitabine), although equivalence cannot be claimed due to the wide confidence interval and should be interpreted cautiously as not as reliable as a direct comparison. Furthermore, the toxicity for gemcitabine in the CONKO-001 trial appears less than that for 5FU/FA (Neoptolemos et al, 2001, 2004), but a robust assessment of the benefit/risk ratio can only be properly addressed by a concurrently randomised comparison as will be carried out in ESPAC-3.
The RTOG-9704 trial compared pre and postchemoradiation gemcitabine (1000 mg m−2 day−1) to pre and postchemoradiation 5FU (250 mg m−2 day−1 given as a continuous infusion) in patients who had undergone pancreatic resection (Regine et al, 2008). Both arms of the study received 5FU-based chemoradiotherapy (50.4 Gy), with the chemotherapy given for 3 weeks pre- and 12 weeks postchemoradiotherapy (Regine et al, 2008). Analysis was restricted to 442 ‘eligible’ patients out of the total of 538 patients originally recruited. There was no difference in the overall survival between the two arms, but a prospectively powered subgroup analysis of the 380 patients with pancreas head cancer revealed a reduction in the risk of death for patients in the gemcitabine-based chemoradiation arm (HR=0.79; 95% CI=0.63–0.99; P=0.047). The conclusions of the ESPAC-1 trial and subsequent meta-analyses with other adjuvant trials suggest that there is no good clinical evidence for the use of chemoradiation in pancreatic cancer in the adjuvant setting (Neoptolemos et al, 2001, 2004; Stocken et al, 2005) or in patients with locally advanced disease (Yip et al, 2006; Sultana et al, 2007a, 2007b), and more recent results are conflicting (Chauffert et al, 2008; Loehrer et al, 2008). The apparent failure of chemoradiation in pancreatic cancer may be ascribed to interference of systemic chemotherapy scheduling and/or significant biological effects, such as the prometastasizing effects of ionising radiation (Biswas et al, 2007).
In conclusion, the current evidence supports the continued use of adjuvant 5FU/FA for treating pancreatic cancer. The results of the ESPAC-3(v2) trial will determine whether gemcitabine is superior or not to this treatment.
References
Biswas S, Guix M, Rinehart C, Dugger TC, Chytil A, Moses HL, Freeman ML, Arteaga CL (2007) Inhibition of TGF-beta with neutralizing antibodies prevents radiation-induced acceleration of metastatic cancer progression. J Clin Invest 117 (5): 1305–1313
Bucher H, Guyatt G, Griffith L, Walter S (1997) The results of direct and indirect treatment comparisons in meta-analysis of randomised controlled trials. J Clin Epidemiol 50 (6): 683–691
Chauffert B, Mornex F, Bonnetain F, Rougier P, Mariette C, Bouché O, Bosset JF, Aparicio T, Mineur L, Azzedine A, Hammel P, Butel J, Stremsdoerfer N, Maingon P, Bedenne L (2008) Phase III trial comparing intensive induction chemoradiotherapy (60 Gy, infusional 5-FU and intermittent cisplatin) followed by maintenance gemcitabine with gemcitabine alone for locally advanced unresectable pancreatic cancer. Definitive results of the 2000–01 FFCD/SFRO study. Ann Oncol 19 (9): 1592–1599
Loehrer PJ, Powell ME, Cardenes HR, Wagner L, Brell JM, Ramanathan RK, Crane CH, Alberts SR, Benson AB (2008) A randomized phase III study of gemcitabine in combination with radiation therapy versus gemcitabine alone in patients with localized, unresectable pancreatic cancer: E4201. J Clin Oncol ASCO annual meeting proceedings (post-meeting edition). vol 26, no. 15S (20 May Supplement): 4506)
Neoptolemos JP, Dunn JA, Stocken DD, Almond J, Link K, Beger H, Bassi C, Falconi M, Pederzoli P, Dervenis C, Fernandez-Cruz L, Lacaine F, Pap A, Spooner D, Kerr DJ, Friess H, Buchler MW, European Study Group for Pancreatic Cancer (2001) Adjuvant chemoradiotherapy and chemotherapy in resectable pancreatic cancer: a randomised controlled trial. Lancet 358 (9293): 1576–1585
Neoptolemos JP, Stocken DD, Friess H, Bassi C, Dunn JA, Hickey H, Beger H, Fernandez-Cruz L, Dervenis C, Lacaine F, Falconi M, Pederzoli P, Pap A, Spooner D, Kerr DJ, Buchler MW, European Study Group for Pancreatic Cancer (2004) A randomized trial of chemoradiotherapy and chemotherapy after resection of pancreatic cancer. New Engl J Med 350 (12): 1200–1210
Neuhaus P, Riess H, Post S, Gellert K, Ridwelski K, Schramm H, Zuelke C, Fahlke J, Langrehr J, Oettle H (2008) CONKO-001: final results of the randomized, prospective, multicenter phase III trial of adjuvant chemotherapy with gemcitabine versus observation in patients with resected pancreatic cancer (PC). J Clin Oncol (2008 ASCO annual meeting proceedings (post-meeting edition). vol 26, no. 15S (20 May Supplement): LBA4504)
Oettle H, Post S, Neuhaus P, Gellert K, Langrehr J, Ridwelski K, Schramm H, Fahlke J, Zuelke C, Burkart C, Gutberlet K, Kettner E, Schmalenberg H, Weigang-Koehler K, Bechstein WO, Niedergethmann M, Schmidt-Wolf I, Roll L, Doerken B, Riess H (2007) Adjuvant chemotherapy with gemcitabine vs observation in patients undergoing curative-intent resection of pancreatic cancer: a randomized controlled trial. JAMA 297 (3): 267–277
Regine WF, Winter KW, Abrams R, Safran H, Hoffman JP, Konski A, Benson AB, Macdonald JS, Kudrimoti MR, Fromm ML, Haddock MG, Schaefer P, Willett CG, Rich TA (2008) Fluorouracil vs gemcitabine chemotherapy before and after fluorouracil-based chemoradiation following resection of pancreatic adenocarcinoma: a randomized controlled trial. JAMA 299 (9): 1019–1026
Stocken DD, Büchler MW, Dervenis C, Bassi C, Jeekel H, Klinkenbijl JH, Bakkevold KE, Takada T, Amano H, Neoptolemos JP (2005) Meta-analysis of randomised adjuvant therapy trials for pancreatic cancer. Br J Cancer 92 (8): 1372–1381
Sultana A, Tudur Smith C, Cunningham D, Starling N, Neoptolemos JP, Ghaneh P (2007a) Meta-analyses of chemotherapy for locally advanced and metastatic pancreatic cancer. J Clin Oncol 25 (18): 2607–2615
Sultana A, Tudur Smith C, Cunningham D, Starling N, Tait D, Neoptolemos JP, Ghaneh P (2007b) Systematic review, including meta-analyses, on the management of locally advanced pancreatic cancer using radiation/combined modality therapy. Br J Cancer 96 (8): 1183–1190
Yip D, Karapetis C, Strickland A, Steer CB, Goldstein D (2006) Chemotherapy and radiotherapy for inoperable advanced pancreatic cancer, (Cochrane database of systematic reviews, issue 3. Article no.: CD002093.DOI:10.1002/14651858.CD002093. pub2)
Acknowledgements
This study was presented on behalf of the members of the European Study Group for Pancreatic Cancer and contributors to the ESPAC-1 and ESPAC-3 adjuvant trials in pancreatic cancer. The study was funded by Cancer Research UK; plus the Fonds de Recherche de la Société Nationale Française de Gastroentérologie; the Consorzio Studi Universitari di Verona, Cariverona and the Ministero Università e Ricerca Scientifica e Tecnologica (Cofin 9906195987) Rome, Italy; Associazione Italiana Ricerca Cancro (AIRC) Milan, Italy; European Community Grant BIOMED 2 CE-contract no. BMH4-CT98-3805; National Cancer Institute, Canada; and Medical Research Council, Australia.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-NoDerivs 3.0 License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/.
About this article
Cite this article
Neoptolemos, J., Stocken, D., Tudur Smith, C. et al. Adjuvant 5-fluorouracil and folinic acid vs observation for pancreatic cancer: composite data from the ESPAC-1 and -3(v1) trials. Br J Cancer 100, 246–250 (2009). https://doi.org/10.1038/sj.bjc.6604838
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6604838
Keywords
This article is cited by
-
Adjuvant Chemoradiotherapy in Resected Pancreatic Ductal Adenocarcinoma: Where Does the Benefit Lie? A Nomogram for Risk Stratification and Patient Selection
Journal of Gastrointestinal Surgery (2022)
-
Plasma biomarkers for prediction of early tumor recurrence after resection of pancreatic ductal adenocarcinoma
Scientific Reports (2021)
-
Incorporating competing risk theory into evaluations of changes in cancer survival: making the most of cause of death and routinely linked sociodemographic data
BMC Public Health (2020)
-
Prognostic value of 18F-FDG PET /CT metabolic parameters in patients with locally advanced pancreatic Cancer treated with stereotactic body radiation therapy
Cancer Imaging (2020)
-
The identification of candidate effective combination regimens for pancreatic cancer using the histoculture drug response assay
Scientific Reports (2020)