Abstract
The stomach is the main digestive organ in humans. Patients with gastric cancer often develop digestive problems, which result in poor nutrition. Nutritional status is closely related to postoperative complications and quality of life (QoL) in patients with gastric cancer. The controlling nutritional status (CONUT) score is a novel tool to evaluate the nutritional status of patients. However, the relationship of the CONUT score with postoperative complications, QoL, and psychological status in patients with gastric cancer has not been investigated. The present follow-up study was conducted in 106 patients who underwent radical gastrectomy in our hospital between 2014 and 2019. The CONUT score, postoperative complications, psychological status, postoperative QoL scores, and overall survival (OS) of patients with gastric cancer were collected, and the relationship between them was analyzed. A significant correlation was observed between the CONUT score and postoperative complications of gastric cancer (P < 0.001), especially anastomotic leakage (P = 0.037). The multivariate regression analysis exhibited that the CONUT score (P = 0.002) is an independent risk factor for postoperative complications. The CONUT score was correlated with the state anxiety questionnaire (S-AI) for evaluating psychological status (P = 0.032). However, further regression analysis exhibited that the CONUT score was not an independent risk factor for psychological status. Additionally, the CONUT score was associated with postoperative QoL. The multivariate regression analysis exhibited that the CONUT score was an independent risk factor for the global QoL (P = 0.048). Moreover, the efficiency of CONUT score, prognostic nutrition index, and serum albumin in evaluating complications, psychological status, and QoL was compared, and CONUT score was found to outperform the other measures (Area Under Curve, AUC = 0.7368). Furthermore, patients with high CONUT scores exhibited shorter OS than patients with low CONUT scores (P = 0.005). Additionally, the postoperative complications (HR 0.43, 95% CI 0.21–0.92, P = 0.028), pathological stage (HR 2.26, 95% CI 1.26–4.06, P = 0.006), and global QoL (HR 15.24, 95% CI 3.22–72.06, P = 0.001) were associated with OS. The CONUT score can be used to assess the nutritional status of patients undergoing gastric cancer surgery and is associated with the incidence of postoperative complications and QoL.
Similar content being viewed by others
Introduction
Gastric cancer has become a common malignant disease, with high incidence and mortality in modern China because of the accelerated pace of life and dietary changes1. Approximately 0.48 million new cases of gastric cancer are reported annually in China. The mortality rate of gastric cancer is second only to lung cancer and colorectal cancer2.
The stomach is the main digestive organ of the human body3. Patients with gastric cancer often experience indigestion symptoms such as stomachache, abdominal distension, nausea, and vomiting, which affect food intake. Therefore, patients with gastric cancer are more likely to have malnutrition than patients with other malignant tumors4. Perioperative malnutrition may increase the incidence of postoperative complications and affect the quality of life (QoL), psychological status, and OS of patients. The preoperative nutritional status of patients must be accurately evaluated and the appropriate nutritional intervention be administered to patients with poor nutritional status to minimize the incidence of postoperative complications and improve the survival rate and QoL of patients with gastric cancer5,6,7. Malnutrition and malignant tumors form a vicious circle where one promotes the other.
An increasing number of clinicians have realized the significance of nutrition in patients with gastric cancer. Therefore, the nutritional status of patients with gastric cancer must be accurately assessed. Nutrition evaluation systems such as NRS2002 and patient-generated subjective global assessment (PG-SGA) are widely used in the clinic for patients with tumors. However, these assessment methods have significant drawbacks due to the tedious, complex, time-consuming, and subjective processes. First, it is limited by the memory and knowledge level of patients; several patients cannot recall and provide the nutritional status accurately. Second, the subjective evaluation of doctors affects the accuracy of conclusions. PG-SGA is associated with similar limitations. Moreover, traditional nutritional assessment tools are subjective and complex, making it difficult for general clinicians to accurately evaluate the nutritional status of patients and efficacy of nutritional interventions. Therefore, the present study attempted to establish a simple and objective evaluation method.
The controlling nutritional status (CONUT) score is an objective nutrition evaluation index based on serum albumin (ALB), total cholesterol, and lymphocyte count. The nutrition score of patients can be easily obtained by delineating the score range of these indices and has a superior evaluation effect on the nutritional status of patients with cancers8. The CONUT score ranges between 0 and 9, and it more accurately reflects the effect of nutritional treatment than other evaluation systems. It is helpful in the perioperative patient management, diagnosis, and treatment planning. The laboratory results of this score are easy to obtain, the evaluation process is simple, and the clinical use of this score is obviously more convenient than that of other tools. The CONUT score was shown to be critical in the nutritional evaluation of patients with gastrointestinal or pulmonary tumors9. However, limited evidence is available to confirm its accuracy. Therefore, the present retrospective study attempted to clarify whether the CONUT score could accurately assess the preoperative nutritional status of patients with gastric cancer and its association with postoperative complications, QoL, and psychological status.
Patients and methods
Statements
The use of clinical data and other follow up procedure in this study were approved by the Human Ethics Review Committee of Shaanxi Provincial People's Hospital (MEC code: SPPH-LLBG-17-3.2).
All participants gave informed consent to the research, allowed access to their clinical data, agreed to receive follow-up and questionnaire surveys, and signed an informed consent form which based on CIOMS guidelines.
Patients
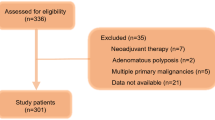
The present study extracted the data of 168 patients, aged more than 18 years, with gastric cancer who underwent gastric cancer-related surgery for the first time from 2014 to 2019 in Shaanxi Provincial People's Hospital. Patients with incomplete data and those who could not be followed up were excluded from the study. Finally, the data of 106 patients were collected to study the correlation of the preoperative CONUT score with postoperative complications, psychological status, and QoL of patients with gastric cancer. The state–trait anxiety inventory (STAI) was used to measure the psychological state and anxiety level of patients. EORTC QLQ-C30 (version 3) was used to evaluate the postoperative QoL of patients.
Data were extracted from medical records, and telephone and web follow-ups were also conducted. The median follow-up period was 30 months (range 7–64 months).
Methods
All methods in this study were carried out in accordance with relevant guidelines and regulations of Shaanxi Provincial People's Hospital.
CONUT score, complications, and other scoring systems
According to the CONUT score items, data on the lymphocyte count, ALB, and total cholesterol levels of patients with gastric cancer were collected within 2 weeks before the surgical procedure, whereas the data on carcinoembryonic antigen (CEA) and carbohydrate antigen 19-9 (CA19-9) levels were collected within 1 month before the operation. The CONUT score was calculated, and all the patients were divided into low CONUT (CONUT < 5) and high CONUT groups (CONUT ≥ 5), with a median score of 5 (range 3–9).
Surgical methods included both laparoscopy and open surgery. The resection range included procedures such as total gastrectomy, subtotal gastrectomy, and distal gastrectomy. Common complications included pulmonary infection, bleeding, anastomotic leakage, anastomotic stenosis, organ failure, severe systemic infection, surgical incision or anastomotic infection, and vascular events (thrombosis). Simultaneously, the classification of surgical complications was determined according to the Clavien–Dindo classification10. We only sorted out the data of the grades II–V complications as the complications of grade I were mild and had little impact on the prognosis.
The postoperative psychological status of the patients was assessed using the STAI (STAI-Formy, S-AI/T-AI). STAI comprises the following two subscales: state anxiety questionnaire (S-AI) and trait anxiety questionnaire (T-AI), each with 20 items. Half of the S-AI (items 1–20) are items describing negative emotions, whereas the other half are items describing positive emotions. These items can be used to evaluate state anxiety under stress. In T-AI (items 21–40), 11 items are negative emotion items, whereas 9 items are positive emotion items. These items are used to assess the frequent and perennial emotional experiences of people.
The EORTC QLQ-C30 (version 3) was used to evaluate the postoperative QoL. The QLQ-C30 contains 30 items, which can be divided into 15 areas, including 5 functional areas (physical function, role function, emotional function, cognitive function, and social function), 3 symptom areas (fatigue, pain, nausea, and vomiting), 1 global health status or QoL area, and 6 single items. High scores in the functional and overall health status fields indicate better functional status and life quality, whereas high scores in the symptom field indicate more symptoms or problems (a lower life quality). Therefore, the raw QLQ-C30 scores were transformed into standard scores for further analysis.
Because of the randomness of remote follow-up and the uncertainty of psychological investigation, a series of strict standards were formulated to minimize the interference factors in the follow-up process under the existing conditions. The content of follow-up was determined in advance, standardized instructions were formulated, and staff were designated in a quiet environment to follow-up from 9 a.m. to 11 a.m., 3–6 p.m., and 7 p.m. to 9 p.m. Each patient was explained the purpose and content of the follow-up and the time required for the same. The study was initiated only after the patient informed consent for the same. We helped the patients recall the psychological changes before operation and the postoperative influence. Several remedial strategies were developed to avoid communication errors and ensure the efficiency of follow-up.
To better assess the predictive value of the CONUT score, two classical indicators of nutritional assessment, namely the prognostic nutritional index (PNI) and ALB content, were introduced for comparison. The experimental flow is illustrated in Fig. 1.
Statistical analysis
All data were analyzed using Excel 2019 (Microsoft, Redmond, WA, USA) and the SPSS Statistics software, versions 22.0 and 26.0 (IBM Corporation, Armonk, NY, USA). P value < 0.05 was considered statistically significant.
Continuous variables are expressed as median (quartile range) or mean ± standard deviation. Classification variables are represented as numbers (%). The t test was used to assess differences in continuous variables such as patient age, length of stay, CA19-9, and STAI. Chi-square test or Fisher's exact test was used to analyze and compare categorical variables such as sex, tumor stage, and complications. Logistics regression analysis was used to analyze whether the CONUT score is an independent risk factor for complications, STAI, and EORTC QLQ-C30. COX regression was used to analyze the relationship between CONUT score and OS. An ROC curve was used to compare the predictive values of CONUT, PNI, and ALB.
Results
Patient characteristics
The median age of the patients was 67 years (43–85 years). According to the World Health Organization age classification criteria, the patients were divided into two groups, namely < 60 years old and ≥ 60 years old. A total of 44 patients (41.5%) died by the time of follow-up. Finally, the study group comprised 84 men (79.2%) and 22 women (20.8%). Of the 106 patients, 17 patients (16%) were in pathology stage I, 20 patients (18.9%) were in stage II, 57 patients (53.8%) were in stage III, and 12 patients (11.3%) were in stage IV as per the tumor, nodes, and metastases (TNM) staging criteria of the National Comprehensive Cancer Network. The chi-square test indicated no correlation between the CONUT score and TNM stage. However, sex (P = 0.016), survival time (P = 0.005), CA19-9 (P = 0.021), and surgical resection range (P = 0.024) were found to be significantly correlated with the CONUT score. Postoperative complications were observed in 39 patients (36.8%). A significant association was observed between CONUT score and postoperative complications (P < 0.001) (Table 1).
Correlation between CONUT score and postoperative complications
Gastric cancer exhibits several postoperative complications such as pulmonary infection, bleeding, anastomotic leakage, and anastomotic stenosis. A significant correlation was observed between anastomotic leakage and CONUT score (P = 0.037). The severity of complications can be divided into the following 5 grades: Grade I: does not require medical and surgical treatment; Grade II: requires medication, blood transfusion, or total parenteral nutrition; Grade III: requires surgery and endoscopy; Grade IV: exhibits life-threatening complications; Grade V: patient dies. The relationship between the complication grade and CONUT score was further analyzed. Grade II complications were found to be significantly correlated with the CONUT score (P = 0.004) (Table 2).
Stratified analysis based on tumor stage showed that patients with high CONUT scores in TNM stage I patients were prone to postoperative complications of grade II (P = 0.023) (Table 3).
Risk factors for postoperative complications
The CONUT score (P < 0.001), PNI (P = 0.05), ALB (P = 0.004), and pathological stage (P = 0.004) were found to be significantly correlated with postoperative complications (Table 4).
Independent risk factors of complications
To further analyze the independent risk factors for postoperative complications, we performed univariate and multivariate analyses of the CONUT score, PNI, and other indicators which affected complications. The CONUT score (HR 0.15, 95% CI 0.06–0.55, P = 0.002) was demonstrated to be an independent risk factor for postoperative complications (Table 5).
Relationship of CONUT score with psychological status
Nutritional status has been reported to be related to postoperative psychological status. Therefore, STAI was used to evaluate postoperative psychological status, and the relationship between CONUT score and STAI was analyzed. The S-AI score, which reflects the anxiety in the postoperative stress state, was found to be significantly correlated with the CONUT score (P = 0.032) (Table 6). However, the T-AI score, which reflects emotional experiences, demonstrated no obvious correlation with the CONUT score (P = 0.058).
The results of stratified analysis based on TNM staging showed that stage III patients with high CONUT scores had higher S-AI scores (P = 0.02) (Table 7). It was suggested that stage III patients with high CONUT scores were more prone to anxiety.
Independent STAI risk factors
Logistic regression analysis was conducted to determine whether the CONUT score is an independent risk factor for the STAI score. However, the CONUT score was not found to be an independent risk factor for both the S-AI (Table 8) and T-AI scores (Table 9).
Relationship of CONUT score with QoL
The nutritional status has been reported to be associated with postoperative QoL. Therefore, EORTC QLQ-C30 was used to evaluate postoperative QoL. Most of the postoperative QoL assessment sub-items were found to be significantly correlated with the CONUT score (Table 10).
In addition, we analyzed the relationship between CONUT scores and preoperative QoL. The CONUT score and preoperative QoL in "Nausea and Vomit (P < 0.001), Appetite loss (P < 0.001), and Diarrhea (P = 0.002)" had significant relationship (Table 11).
The results of the stratified analysis based on tumor stage showed that the postoperative emotional function (P = 0.0225), cognitive function (P = 0.025), global QoL (P = 0.044) and dyspnea (P = 0.03) of patients in stage III were significantly correlated with the CONUT score (Table 12).
Independent risk factors for postoperative QoL
The independent risk factors for QoL after gastric cancer surgery were analyzed. Of the several QoL sub-items, the global QoL is the most representative. Therefore, it was used to represent the QoL for the subsequent multivariate regression analysis. The pathological stage (HR 0.13, 95% CI 0.03–0.67, P = 0.014), CONUT (HR 3.14, 95% CI 1.01–9.74, P = 0.048), and surgical methods (HR 3.13, 95% CI 1.15–8.54, P = 0.026) were found to be independent risk factors for general health (Table 13).
Comparison of the values of CONUT score, PNI, and ALB
Although the CONUT score was found to be significantly correlated with the postoperative complications, psychological status, and QoL, it must be compared with other nutritional assessment tools. Therefore, the predictive validity of the CONUT score, PNI, and ALB was compared. The CONUT score was demonstrated to be superior to other nutrition assessment methods, especially for the prediction of complications (AUC = 0.7368) (Fig. 2).
Associations of CONUT score with OS
Studies have reported11 that the CONUT score is closely related to OS of patients with various cancers. Therefore, the univariate and multivariate regression analyses were performed to determine whether the CONUT score is an independent risk factor for OS in patients with gastric cancer after surgery. The univariate analysis exhibited that the postoperative complications (HR 0.22, 95% CI 0.12–0.42, P < 0.001), pathological stage (HR 3.69, 95% CI 2.23–6.11, and P < 0.001), and S-AI (HR 0.38, 95% CI 0.19–0.76, P = 0.006), T-AI (HR 0.43, 95% CI 0.23–0.83, P = 0.012), and QoL scores are significantly correlated with OS. And the multivariate analysis exhibited complications (HR 0.43, 95% CI 0.21–0.92, P = 0.028), pathological stage (HR 2.26, 95% CI 1.26–4.06, P = 0.006), and global QoL scores (HR 15.24, 95% CI 3.22–72.06, P = 0.001) as the independent factors for OS (Table 14).
Discussion
Although several tumor-related nutrition assessment tools have emerged in the past decades, the application of some of these tools is still controversial and criticized in practical clinical work12. NRS2002 and other evaluation systems require patients to review body weight changes. However, reviewing the weight changes before onset is difficult for elderly patients as they are usually ignorant of weight changes and may have difficulty remembering. Anthropometric parameters are indispensable in NRS2002 and other classical nutritional evaluation methods. However, these assessment tools have limitations and are ineffective in nutritional screening and assessment of patients with malignant tumors who are extremely weak or edematous as pleural fluid and ascites affect the body weight. Additionally, the sebum thickness of patients with edema cannot accurately reflect the nutritional status; however, it will adversely affect the final nutritional score. Although PG-SGA is an improved nutrition evaluation treatment for patients with cancer, its design cannot accurately reflect the nutritional status of patients with gastric cancer. For example, although breast cancer and stomach cancer are both malignant tumors, the food intake and absorption in patients with gastric cancer is obviously poorer than that in patients with breast cancer. Thus, the same evaluation system would be inaccurate. Additionally, nutrition evaluation systems such as NRS2002 and PG-SGA are too simple to classify malnutrition, and thus are unsuitable for the dynamic evaluation of malnutrition and the effect of nutritional intervention.
Some scholars believe that changes in the internal environment can not only reflect the nutritional status but also help evaluate the risk of postoperative complications13. Several subjective parameters are present in clinical nutrition evaluation methods such as NRS2002 that affect the accuracy of the evaluation14. The application of CONUT score may open a new door for nutritional assessment and postoperative complication prediction. The CONUT score is an objective evaluation criterion, which is completely based on laboratory parameters. Lymphocyte count is a direct observation index of inflammatory response in patients and also reflects the status of immune surveillance to some extent15. ALB can effectively reflect the nutritional status of patients, and it is also related to the liver function reserve and release of inflammatory cytokines from tumor cells16. As the main component of the cell membrane, total cholesterol is involved in various signal pathways in tumor pathogenesis and development17. Our results also confirm that patients with high CONUT scores are more likely to have postoperative complications, and the finding is consistent with those of other studies18. Compared with other nutrition evaluation systems widely used in clinical practice such as NRS2002 and PNI, CONUT score is more accurate and convenient for nutritional evaluation due to the objective and dynamic laboratory results.
The present study exhibited no significant correlation of age, survival status, and length of hospital stay with the CONUT score. This finding is in contrast with that of a study on prognosis of elderly patients with colorectal cancer by Ahiko18, which reported that age is significantly correlated with the CONUT score. This difference in research results may be attributed to differences in the subject and age stratification between the two studies. The increasing age results in a gradual decline in body function, leading to poor nutritional status. The role of age in the CONUT score was affected due to the large age span of observers enrolled in our study. Other studies9,19,20 have suggested that sex is not associated with the CONUT score. However, our results exhibited that sex is also one of the factors influencing the CONUT score. Differences in the dietary structure and basic metabolic level between men and women in China may affect the nutritional status to a certain extent. CA19-9 is a marker of malignant tumors such as gastrointestinal malignancies and ovarian cancer, and it is also increased in some chronic inflammatory states21. Some studies have observed that CA19-9 has a certain correlation with glucose and lipid metabolism22. Therefore, the correlation between CA19-9 and CONUT score can be easily understood23.
Postoperative complications have received great attention. Some scholars have observed that the CONUT scores of patients with breast cancer, lung cancer, and colorectal cancer are related to postoperative complications18,24. Consistent with their findings, we observed a strong correlation between the CONUT score and postoperative grade II complications such as anastomotic leakage. Malnutrition affects the healing and repair of tissues in case of anastomotic leakage. Studies have proved that the incidence of complications such as anastomotic leakage can be greatly reduced by improving the nutritional status of patients25. In our study, the CONUT score, PNI, or ALB were strongly associated with postoperative complications, indicating that the nutritional status is a crucial factor affecting the surgical complications. Through univariate and multivariate regression analyses, we observed that the CONUT score is an independent risk factor for postoperative complications, indicating that CONUT score could reflect the relationship between nutritional status and postoperative complications.
The psychological status of patients with cancers has also been receiving considerable attention. Numerous patients with malignant tumors exhibit depression and anxiety, which affects the prognosis of the disease26. Studies have exhibited that patients with malnutrition are more likely to develop depression and anxiety27,28. Therefore, we used the STAI questionnaire to assess the psychological state of patients with gastric cancer after surgery. Patients with a high preoperative CONUT score also exhibited a high postoperative S-AI score, suggesting that poor preoperative nutrition will increase the anxiety and depression in the short term after surgery. However, the preoperative CONUT score exhibited no significant correlation with postoperative T-AI, suggesting that preoperative nutritional status had little effect on postoperative long-term psychological state. We further performed a logistics regression analysis and observed that the CONUT score was not an independent risk factor for T-AI and S-AI. Our results suggest that nutritional status is not the main factor that affects the postoperative psychological state of patients and that postoperative psychological anxiety may be more affected by other factors.
Postoperative QoL has also been studied in recent years, and a close correlation of the nutritional status with the QoL has been observed29. Therefore, we evaluated the postoperative QoL in patients with gastric cancer by using EORTC QLQ-C30. The EORTC QLQ-C30 assessed the QoL of patients in terms of function, symptoms, and overall health28 (Global QoL). Patients with a high CONUT score exhibited lower scores for physical function, role function, cognitive function, emotional function, social function, and global QoL than patients with a low CONUT score. Additionally, patients with high CONUT scores exhibited higher scores for fatigue, pain, dyspnea, and financial difficulty than patients with low CONUT scores. According to the scoring criteria of the EORTC QLQ-C30 scale, high scores for the function and global QoL indicate better functional status and life quality, whereas high scores for the symptom area indicate more symptoms or problems (a lower QoL). It also suggests that patients with a high CONUT score are associated with poor QoL. We conducted univariate and multivariate regression analyses and observed that the CONUT score is an independent risk factor for the QoL of patients with gastric cancer after surgery. In addition, we evaluated the relationship between COUNT score and preoperative QoL in patients with gastric cancer. The symptoms of the digestive system are closely related to the CONUT score, but there is no obvious correlation in other aspects. We found that the results of QoL score before surgery were significantly worse than after surgery. Confusion and pain caused by the disease were far more influential than the nutritional status. Preoperative QoL may be more influenced by the disease itself, while nutrition did not dominate. Several studies have observed that the CONUT score is associated with postoperative OS of patients30. Therefore, we also analyzed the relationship between CONUT score and postoperative OS of patients with gastric cancer. The CONUT score exhibited no significant correlation with OS and could not be used to predict the prognosis of patients. This finding is concurrent with that of other studies31. Predicting the prognosis of patients undergoing gastric cancer surgery is challenging32. The postoperative TNM stage is a decisive factor affecting the prognosis of patients with gastric cancer. Additionally, postoperative complications, accidents, and economic status may affect OS of these patients. Although nutritional status influences postoperative OS, it is not a major determinant.
The present study has certain limitations. The single-center retrospective design of the study may introduce a certain degree of data bias. However, we screened cases strictly and ensured the validity and representativeness of the data as much as possible in the statistical process. Moreover, we attempted to make the questionnaire as detailed as possible in the follow-up process to reduce the loss of effective data. With the increasing geriatric population, the nutritional status of elderly patients has attracted attention. Future studies in elderly patients with a larger sample size would allow the further analysis of the application of the CONUT score.
Conclusion
The CONUT score is a simple and objective measure that can reduce the workload of clinicians. Therefore, it has a certain clinical value in preoperative nutrition assessment of gastric cancer and can be used to predict postoperative complications and QoL.
References
Wei, W. et al. Cancer registration in china and its role in cancer prevention and control. Lancet Oncol. 21, 342–349. https://doi.org/10.1016/S1470-2045(20)30073-5 (2020).
Smyth, E. C., Nilsson, M., Grabsch, H. I., van Grieken, N. C. T. & Lordick, F. Gastric cancer. Lancet 396, 635–648. https://doi.org/10.1016/s0140-6736(20)31288-5 (2020).
Hunt, H. et al. The stomach in health and disease. Gut 10, 1650–1668. https://doi.org/10.1136/gutjnl-2014-307595 (2015).
Hirahara, N. et al. Controlling Nutritional Status (CONUT) as a prognostic immunonutritional biomarker for gastric cancer after curative gastrectomy: a propensity score-matched analysis. Surg. Endosc. 33, 4143–4152. https://doi.org/10.1007/s00464-019-06723-z (2019).
Pisegna, J., Xu, M., Spees, C. & Krok-Schoen, J. Mental health-related quality of life is associated with diet quality among survivors of breast cancer. Support. Care Cancer https://doi.org/10.1007/s00520-020-05698-1 (2020).
Kim, J., Kim, J., Williams, R. & Han, A. The Association of Social Support and Leisure Time Physical Activity With Mental Health Among Individuals With Cancer. Am. J. Health Promot. AJHP https://doi.org/10.1177/0890117120961321 (2020).
Wang, S. et al. Postoperative complications and prognosis after radical gastrectomy for gastric cancer: a systematic review and meta-analysis of observational studies. World J. Surg. Oncol. 17, 52. https://doi.org/10.1186/s12957-019-1593-9 (2019).
Kheirouri, S. & Alizadeh, M. Prognostic potential of the preoperative controlling nutritional status (CONUT) score in predicting survival of patients with cancer: a systematic review. Adv. Nutr (Bethesda, Md.) https://doi.org/10.1093/advances/nmaa102 (2020).
Lee, S. et al. Prediction of postoperative pulmonary complications using preoperative controlling nutritional status (CONUT) score in patients with resectable non-small cell lung cancer. Sci. Rep. 10, 12385. https://doi.org/10.1038/s41598-020-68929-9 (2020).
Clavien, P. A. et al. The Clavien-Dindo classification of surgical complications: Five-year experience. Ann. Surg. 250, 187–196. https://doi.org/10.1097/SLA.0b013e3181b13ca2 (2009).
Ruo, L. et al. The prognostic role of controlling nutritional status scores in patients with solid tumors. Clin. Chim. Acta 474, 155–158. https://doi.org/10.1016/j.cca.2017.09.021 (2017).
Fujiya, K. et al. Preoperative risk factors for postoperative intra-abdominal infectious complication after gastrectomy for gastric cancer using a Japanese web-based nationwide database. Gastric Cancer https://doi.org/10.1007/s10120-020-01083-3 (2020).
Kunisaki, C. et al. Modeling preoperative risk factors for potentially lethal morbidities using a nationwide Japanese web-based database of patients undergoing distal gastrectomy for gastric cancer. Gastric Cancer 20, 496–507. https://doi.org/10.1007/s10120-016-0634-0 (2017).
Etoh, T. et al. Morbidity and mortality from a propensity score-matched, prospective cohort study of laparoscopic versus open total gastrectomy for gastric cancer: Data from a nationwide web-based database. Surg. Endosc. 32, 2766–2773. https://doi.org/10.1007/s00464-017-5976-0 (2018).
Singh, S., Gupta, P., Meena, A. & Luqman, S. Acacetin, a flavone with diverse therapeutic potential in cancer, inflammation, infections and other metabolic disorders. Food Chem. Toxicol. 145, 111708. https://doi.org/10.1016/j.fct.2020.111708 (2020).
Liu, J. et al. The prognostic role of preoperative serum albumin/globulin ratio in patients with bladder urothelial carcinoma undergoing radical cystectomy. Urol. Oncol. 34(484), e481-484.e488. https://doi.org/10.1016/j.urolonc.2016.05.024 (2016).
Haghikia, A. & Landmesser, U. High-density lipoproteins: Effects on vascular function and role in the immune response. Cardiol. Clin. 36, 317–327. https://doi.org/10.1016/j.ccl.2017.12.013 (2018).
Ahiko, Y. et al. Controlling nutritional status (CONUT) score as a preoperative risk assessment index for older patients with colorectal cancer. BMC Cancer 19, 946. https://doi.org/10.1186/s12885-019-6218-8 (2019).
Yoshida, N. et al. Preoperative controlling nutritional status (CONUT) is useful to estimate the prognosis after esophagectomy for esophageal cancer. Langenbecks Arch. Surg. 402, 333–341. https://doi.org/10.1007/s00423-017-1553-1 (2017).
Kuroda, D. et al. Controlling Nutritional Status (CONUT) score is a prognostic marker for gastric cancer patients after curative resection. Gastric Cancer 21, 204–212. https://doi.org/10.1007/s10120-017-0744-3 (2018).
Locker, G. Y. et al. ASCO 2006 update of recommendations for the use of tumor markers in gastrointestinal cancer. J. Clin. Oncol. 24, 5313–5327. https://doi.org/10.1200/jco.2006.08.2644 (2006).
Parhofer, K. G. Interaction between glucose and lipid metabolism: More than diabetic dyslipidemia. Diabetes Metab. J. 39, 353–362. https://doi.org/10.4093/dmj.2015.39.5.353 (2015).
Tokunaga, R. et al. CONUT: a novel independent predictive score for colorectal cancer patients undergoing potentially curative resection. Int. J. Colorectal Dis. 32, 99–106. https://doi.org/10.1007/s00384-016-2668-5 (2017).
Kang, N. et al. Mediating and moderating factors of adherence to nutrition and physical activity guidelines, breastfeeding experience, and spousal support on the relationship between stress and quality of life in breast cancer survivors. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph17207532 (2020).
Ryo, S. et al. The controlling nutritional status score serves as a predictor of short- and long-term outcomes for patients with stage 2 or 3 gastric cancer: Analysis of a multi-institutional data set. Ann. Surg. Oncol. 26, 456–464. https://doi.org/10.1245/s10434-018-07121-w (2019).
Daniel, S., Azuero, A., Gutierrez, O. & Heaton, K. Examining the relationship between nutrition, quality of life, and depression in hemodialysis patients. Qual. Life Res. https://doi.org/10.1007/s11136-020-02684-2 (2020).
Salm, S. et al. Mental disorders and utilization of mental health services in newly diagnosed cancer patients: An analysis of German health insurance claims data. Psychooncology https://doi.org/10.1002/pon.5579 (2020).
Carreira, H. et al. Quality of life and mental health in breast cancer survivors compared with non-cancer controls: A study of patient-reported outcomes in the United Kingdom. J. Cancer Survivorship Res. Pract. https://doi.org/10.1007/s11764-020-00950-3 (2020).
Mehdorn, A. et al. Long-term, health-related quality of life after open and robot-assisted Ivor-Lewis procedures—A propensity score-matched study. J. Clin. Med. https://doi.org/10.3390/jcm9113513 (2020).
Liang, R. F., Li, J. H., Li, M., Yang, Y. & Liu, Y. H. The prognostic role of controlling nutritional status scores in patients with solid tumors. Clin. Chim. Acta 474, 155–158. https://doi.org/10.1016/j.cca.2017.09.021 (2017).
Mimatsu, K., Fukino, N., Ogasawara, Y., Saino, Y. & Oida, T. Utility of inflammatory marker- and nutritional status-based prognostic factors for predicting the prognosis of stage IV gastric cancer patients undergoing non-curative surgery. Anticancer Res 37, 4215–4222. https://doi.org/10.21873/anticanres.11812 (2017).
Dias, A. et al. Prediction scores for complication and recurrence after multivisceral resection in gastric cancer. Eur. J. Surg. Oncol. 46, 1097–1102. https://doi.org/10.1016/j.ejso.2020.01.014 (2020).
Acknowledgements
We would like to thank TopEdit (www.topeditsci.com) for its linguistic assistance during the preparation of this manuscript.
Funding
This study was supported by: Key R&D Projects in Shaanxi Province (2019ZDLSF02-09-01); Shaanxi Provincial Innovation capability support Plan Project (2019GHJD-14); The Education Department of Shaanxi Province serves the Local Special Plan Project (18JC027); Natural Science Basic Research Program of Shaanxi Province (2020JQ-947).
Author information
Authors and Affiliations
Contributions
Conceptualization: Y.P. and X.D.; Data curation: Q.X., S.S. and B.X.; Formal analysis: B.D. and X.L.; Investigation: S.L.; Methodology: J.Z.; Project administration: X.L. and H.Q.; Writing—original draft: Q.X. and X.L.; Writing—review & editing: Q.X. and X.L.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Xiao, Q., Li, X., Duan, B. et al. Clinical significance of controlling nutritional status score (CONUT) in evaluating outcome of postoperative patients with gastric cancer. Sci Rep 12, 93 (2022). https://doi.org/10.1038/s41598-021-04128-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-04128-4
This article is cited by
-
Prognostic potential of nutritional risk screening and assessment tools in predicting survival of patients with pancreatic neoplasms: a systematic review
Nutrition Journal (2024)
-
Comparative analysis of four nutritional scores predicting the incidence of MACE in older adults with acute coronary syndromes after PCI
Scientific Reports (2023)
-
Preoperative low absolute and relative handgrip strength as predictors of postoperative short-term outcomes: a prospective study based on patients aged 60 years and older with gastric cancer
European Geriatric Medicine (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.