Abstract
Background:
Hyperthermic intraperitoneal chemotherapy (HIPEC) is advised as a treatment option for epithelial ovarian cancer (EOC) with peritoneal carcinomatosis. This study was designed to define the pharmacokinetics of cisplatin (CDDP) and paclitaxel (PTX) administered together during HIPEC.
Methods:
Thirteen women with EOC underwent cytoreductive surgery (CRS) and HIPEC, with CDDP and PTX. Blood, peritoneal perfusate and tissue samples were harvested to determine drug exposure by high-performance liquid chromatography and matrix-assisted laser desorption ionization imaging mass spectrometry (IMS).
Results:
The mean maximum concentrations of CDDP and PTX in perfusate were, respectively, 24.8±10.4 μg ml−1 and 69.8±14.3 μg ml−1; in plasma were 1.87±0.4 μg ml−1 and 0.055±0.009 μg ml−1. The mean concentrations of CDDP and PTX in peritoneum at the end of HIPEC were 23.3±8.0 μg g−1 and 30.1±18.3 μg−1g−1, respectively. The penetration of PTX into the peritoneal wall, determined by IMS, was about 0.5 mm. Grade 3–4 surgical complications were recorded in four patients, five patients presented grade 3 and two patients presented grade 4 hematological complications.
Conclusions:
HIPEC with CDDP and PTX after CRS is feasible with acceptable morbidity and has a favorable pharmacokinetic profile: high drug concentrations are achieved in peritoneal tissue with low systemic exposure. Larger studies are needed to demonstrate its efficacy in patients with microscopic postsurgical residual tumours in the peritoneal cavity.
Similar content being viewed by others
Main
Hyperthermic intraperitoneal chemotherapy (HIPEC) is used for early loco regional intraoperative treatment and is performed immediately after completing cytoreductive surgery (CRS). The combination of CRS with HIPEC can improve the survival of patients with pseudo-myxoma peritonei, malignant peritoneal mesothelioma or peritoneal carcinomatosis (PC) from advanced abdomino-pelvic tumours (Verwaal et al, 2008; Yang et al, 2011; Ansaloni et al, 2012; Baratti et al, 2012; Chua et al, 2012; Coccolini et al, 2013b; Coccolini et al, 2014). Large randomised clinical trials are ongoing to assess the clinical efficacy of HIPEC in epithelial ovarian cancer (EOC) (Coccolini et al, 2013a).
Convincing data are available on the synergism between heat and the activity of many antineoplastic drugs against tumour cells growing in vitro (Huang et al, 1994; Urano et al, 1999), and pharmacokinetic data provide a rational backing for HIPEC, but more pharmacological data and comparative efficacy studies are certainly still needed (Elias et al, 2007; Cashin et al, 2012). The pharmacokinetics of drugs administered during HIPEC after CRS have been established for many different anticancer agents (Van der Speeten et al, 2012), including mainly cisplatin (CDDP) (Cho et al, 1999; Cashin et al, 2012; Cashin et al, 2013; Zivanovic et al, 2014) and paclitaxel (PTX) (de Bree et al, 2008), which are among the most effective against ovarian cancer. In these patients with PC, good efficacy results was seen when the two drugs were infused together during HIPEC (Ansaloni et al, 2012). However, the pharmacokinetics of these drugs have been investigated after intraperitoneal administration associated to hyperthermia only as single agents and not in combination, so we cannot exclude pharmacokinetic drug interaction between them.
To improve our knowledge on this point, we investigated the pharmacokinetics of CDDP and PTX combined during HIPEC after CRS in patients with EOC and PC by determining both drug concentrations in plasma, perfusate and peritoneal tissue. It is especially important to understand the penetration of drugs in peritoneal tissue because human ovarian cancer metastasis are often nested in this tissue and although some information has been published for CDDP (Los et al, 1991; Zivanovic et al, 2014), no data are available for PTX. This lack of information prompted us to investigate by matrix-assisted laser desorption ionization (MALDI) imaging mass spectrometry (IMS) the depth of penetration of PTX in peritoneal tissue.
Materials and methods
Patients
From March 2012 to November 2013, according to the CARPEPACEM protocol, (approved by the Ospedali Riuniti Bergamo, Italy ethical committee), 13 patients with PC from EOC expected to be sensitive to CDDP and PTX were treated by CRS and HIPEC, with both drugs combined. Blood cell count and biochemical liver and renal function tests were in the normal range. The patients’ main characteristics are reported in Table 1. The presence of extra-abdominal or parenchymal metastases was ruled out during the preoperative work-up. Patients’ WHO performance status was >2. Patients mean age was 57 years (s.d.±9.6, median 59 years, range 42–72). Nine patients had primary disease (seven had stage IIIc and two had stage IV for mediastinic lymph-adenopathies) and four recurrent disease. In our patients, the mean peritoneal cancer index, a rating system indicating the extent of metastasis in the peritoneal cavity, was 3.8 (median 4, range 0–7).
The nine patients, where CRS and HIPEC was the primary treatment, have previously been treated with PTX and CDDP or PTX and carboplatin (CBDCA) as systemic neoadjuvant chemotherapy (PTX 175 mg m−2 and CBDCA area under curve (AUC) 5 i.v. schedule, every 21 days): three patients were given six cycles, three others had four and the last one had three cycles. The last chemotherapy on average was 1.3 months (median 1.2, range 1–2) before the HIPEC procedure.
According to the RECIST criteria, four patients exhibited a complete response and the other five exhibited a partial response; the two stage IV patients had regressed to stage IIIc. The response to chemotherapy was evaluated by computed tomography scan (Coccolini et al, 2013a).
The four patients with recurrent disease were treated differently: one underwent CRS and adjuvant systemic PTX+CBDCA chemotherapy (5 cycles) with complete response, and after recurrence 1 year later, was given trabectedin+pegylated doxorubicin systemic chemotherapy (10 cycles), with a partial response before CRS and HIPEC. The other three patients had previously been treated with CRS and adjuvant systemic PTX+CBDCA (five and six cycles) with complete response, and at recurrence no further systemic chemotherapy was scheduled before CRS and HIPEC.
In addition to the 13 EOC patients, one male patient, 43 years old, affected by gastric adenocarcinoma stage IV with peritoneal cancer index 6, was studied only for IMS purposes. This patient met the same inclusion criteria as the other ones and underwent the cytoreductive procedure and HIPEC.
Cytoreductive surgery and HIPEC
The technique of CRS and HIPEC has been previously described (Ansaloni et al, 2012). Peritonectomy was done only for the peritoneal surfaces involved by cancer. The completeness of the cancer resection was assessed at the end of CRS (CC-0, no macroscopic residual; CC-1, residual nodule <2.5 mm; CC-2, residual nodule between 2.5–25 mm; CC-3, residual nodules >25 mm) (Gonzalez-Moreno et al, 2008; Sugarbaker, 2009). The goal of CRS is CC-0/CC-1. The peritoneal cavity was perfused with the open technique using a roller-pump/heat-exchanger (Belmont Hyperthermia Pump). The intraperitoneal temperature during HIPEC was measured with two probes (upper abdomen and pelvis). The system is filled with peritoneal dialysis solution (Baxter, Deerfield, IL, USA). The total volume of the perfusate in litres is calculated by multiplying the body surface area (BSA) by 2.3. BSA was calculated with the following DuBois and DuBois formula: (0.007184 × height (cm)0.725 × weight (kg)0.425) to 2.3 (Wang et al, 1992). The dosages for CDDP and PTX were, respectively, 100 and 175 mg m−2 of BSA. The two drugs were diluted separately in two bags of 500 ml of perfusate. The target inflow temperature varied from 43 °C to 48 °C in order to reach 41–43 °C in the abdomen. HIPEC is done for 90 min during which the surgeon mixes the perfusate continuously within the abdomen. The patient core temperature was monitored and kept below 38.5 °C by cooling devices.
After HIPEC, the perfusate containing chemotherapy was removed and abdominal washing was done. All complications were evaluated and recorded according to the Common Terminology Criteria for Adverse Events v3.0. Anaemia during the first 2 postoperative days was not interpreted as hematological toxicity, but as a result of CRS. A drop in haemoglobin after these first two days is considered systemic toxicity.
Pharmacokinetic study and IMS: sample collection
During perfusion, blood specimens (5 ml) were drawn from a peripheral vein and collected directly into heparinised tubes. The collection times were: pre-perfusion and 30, 60 and 90 min during perfusion. Tubes were centrifuged (2500 rpm, 10 min, 4 °C) within 15 min and plasma was transferred into cryovials. Perfusate was collected 5, 30, 60 and 90 min after the start of perfusion. Abdominal wall peritoneal tissue samples were excised at the end of perfusion.
The samples were stored at −20 °C until analysis, except for the peritoneal tissue taken for IMS (three patients), which were snap frozen in liquid nitrogen and stored at −80 °C.
Pharmacokinetic study: analytical methods
The total concentrations of PTX in plasma, tissue and perfusate sample were determined by high-performance liquid chromatography (HPLC) coupled to ultraviolet detection (λ=230 nm). The analytical reference standard powder of PTX and the internal standard (IS) IDN5390 were generously provided by Indena SPA, Settala (MI), Italy. The methods used were based on our previous publications (Fruscio et al, 2006; Cesca et al, 2009). In brief, 1 ml of plasma was spiked with 0.5 μg of IS and 1 ml of 0.2 M ammonium acetate buffer pH 5, mixed and centrifuged. Supernatants were processed using a Bench Mate Workstation (Zymark, Hopkinton, MA, USA), with Ciano Sep-Pak cartridges for solid-phase extraction (Waters Associates, Milford, MA, USA). Paclitaxel was eluted with 0.1% triethylamine in CH3CN. The eluent was dried under nitrogen, the residue reconstituted in 150 μl of mobile phase and injected into the HPLC system (Alliance 2695, Waters). The chromatography column was a Symmetry C18, 5 μm, 4.6 × 150 mm (Waters). The mobile phase of CH3COONH4 0.01 M pH 5 (50%), CH3CN (40%), CH3OH (10%) was pumped at a flow rate of 1.3 ml min−1. Each study sample was assayed together with a five-point plasma calibration curve at concentrations ranging from 0.05 to 2.5 μg ml−1. The limit of quantification (LOQ) was 0.05 μg ml−1.
For the determination of PTX in peritoneum, tissue samples were homogenised in 0.2 M CH3COONH4 pH 5 (1:2 wt per vol). The homogenate (0.5 ml) was added with 1 μg of IS and extracted with 4 ml of CH3CN. The organic phase was processed and analysed under the same conditions reported above for plasma. Peritoneal tissues obtained before treatment during CRS were used to prepare the calibration curve by the addition of PTX in the range 0.6–30.0 μg g−1. The LOQ was 0.6 μg g−1.
For the determination of PTX in perfusate, 0.1 ml of solution was spiked with 5 μg of IS and extracted with 0.5 ml of CH3CN. The organic phase was dried under nitrogen, the residue was dissolved with 250 μl of mobile phase and analysed as for plasma. Aliquots of perfusate samples without drugs were used to prepare the calibration curve by the addition of PTX in the range 10–100 μg ml−1.
For the analysis of CDDP, tissue, plasma and perfusate samples were processed for total platinum measurement by Atomic Absorption (AA) with an Analyst 600 (Perkin Elmer, Waltham, MA, USA). A sample of 200 μl of plasma or perfusate or 0.2 g of peritoneal tissue was mixed with 400 μl of HNO3:HCl (1:3). After 12 h digestion at room temperature, samples were mixed with 600 μl of bi-distilled water, vortex mixed 30 s and centrifuged at 13 000 rpm for 10 min at 4 °C. The supernatant was injected into the AA instrument (Canta et al, 2011). A calibration curve with platinum standard (Sigma Aldrich, St Louis, MO, USA; lot. 046K1414) was generated in the range 2–200 ng ml−1 (LOQ 2 ng ml−1). The concentration of platinum obtained was expressed as the corresponding CDDP concentration.
The area under the concentration versus time curve (AUC) in plasma was calculated by the trapezoidal rule (WinNonlin 5.0, Pharsight Corporation, Mountain View, CA, USA).
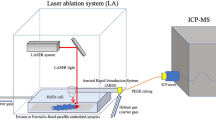
Imaging mass spectrometry
The visualisation of distribution of PTX in peritoneal tissue was determined by IMS according to the method we recently published (Morosi et al, 2013). Frozen tissues were cut into 10-μm-thick sections using a cryo-microtome (Leica Microsystems, Wetzler, Germany) at −20 °C and mounted on a pre-cooled MALDI plate (Opti-TOF 384 Well insert) by standard thaw-mounting techniques. The plate was dried in a vacuum drier at room temperature overnight then sprayed with TiO2 matrix suspension using a BD 180 precision double-action trigger airbrush (Fengda, Prague, Czech Republic) with a 0.20 mm nozzle diameter, with nitrogen at 0.2 atm.
A MALDI 4800 TOF-TOF (AB SCIEX Old Connecticut Path, Framingham, MA 01701, USA) was used, equipped with a 355-nm Nd:YAG laser with a 200 Hz repetition rate, controlled by 4000 Series Explorer software (AB SCIEX Old Connecticut Path). MS spectra were acquired with 20 laser shots at an intensity of 6000 arbitrary units, with a bin size of 1.0 ns, in reflectron negative-ion mode. Images of tissue sections were acquired using the 4800 Imaging Tool software (www.maldi-msi.org, M Stoeckli, Novartis Pharma, Basel, Switzerland), with an imaging raster of 75 × 75 μm by plotting the fragment ion at m/z 284.2 corresponding to the side chain with the amide–acyl group of PTX (Morosi et al, 2013).
Tissue View software 1.1 (AB SCIEX Old Connecticut Path) was used to process and display the ions distribution inside the tumour sections.
Results
Treatment and complications
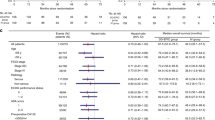
In all patients, CC-0 was obtained. Surgical procedures included: excision of all peritoneal nodules and involved the peritoneum (peritonectomy), hysterectomy (seven patients), bilateral adnexectomy (6), pelvic peritonectomy (12), omentectomy (8), cholecystectomy (9), appendectomy (4), sigmoidectomy (2), right diaphragmatic peritonectomy (5) and left diaphragmatic peritonectomy (3). After CRS, a mean of 3.5 l (median 3.8 l, range 3.5–4.1 l) of perfusate solution was used for HIPEC. The mean dosage administered was 291 mg (median 291, range 263–313 mg) for PTX and 166 mg for CDDP (median 166 mg, range 150–178 mg). Two patients presented grade 4 surgical complications (intestinal perforations) and required re-intervention, two had grade 3 complications (one recto-vaginal phistula necessitating reintervention and one neurogenic urinary bladder requiring long-term catheterisation) (Table 2); five had grade 3 and two patients grade 4 hematological complications (Table 2). There were no deaths perioperatively and during the first 30 postoperative days.
Pharmacokinetic study
Table 3 summarises the main pharmacokinetic results in the 13 patients. For CDDP, the plasma Cmax at 90 min was 1.87±0.4 μg ml−1 with AUC0–90 calculated between T0 and 90 min of 128.5±36.4 μg ml−1*min. PTX was measurable in plasma in 7 of the 13 patients, but only at the end of the perfusion, and the mean concentration was 0.055±0.009 μg ml−1 (0.064±0.010 μmol l−1), range: 0.044–0.068 μg ml−1 (0.051-0.079 μmol l−1). The ratio between perfusate Cmax and plasma Cmax was 1196 and 14 for PTX and CDDP, respectively. In perfusate, PTX was above the cytotoxic threshold level of 0.1 μmol l−1 (Wiernik et al, 1987) throughout the perfusion, whereas plasma levels were lower than the toxic threshold responsible for neutropenia (Figure 1A). Plasma CDDP concentrations were also below the cytotoxic threshold (10 μg ml−1), whereas the drug levels in perfusate was very high during the first hour, then dropped below the threshold by the end of perfusion (9.0±3.1 μg ml−1), though still high enough to inhibit proliferation in 90% of tumour cells in vitro (Royer et al, 2005; Uboldi et al, 2012).
After 90 min of perfusion, both CDDP and PTX achieved high concentrations in peritoneal tissue, respectively of 24.83±10.38 μg g−1 and 30.08±18.31 μg g−1. PTX tissue level at the end of HIPEC was 545 times higher than the plasma Cmax and 362 times higher than the cytotoxic threshold, though there was a wide inter-individual variability (Figure 1B). CDDP concentrations in tissue were 13 times higher than plasma Cmax, equal to the perfusate Cmax and 2.5 times higher than the cytotoxic threshold (Figure 1B).
Paclitaxel penetration in abdominal wall
PTX penetration in peritoneal tissue was assessed by MALDI IMS in two EOC patients (see figure 2: A and B corresponding to 4 and 11) and in a third patient affected by gastric carcinoma (patient C: PTX plasma Cmax 0.061 μg ml−1; PTX perfusate Cmax 67.60 μg ml−1; PTX tissue Cmax 5.4 μg g−1). Figure 2 shows the imaging analysis of one section of peritoneal tissue for each patient. The drug, marked by light blue, was evident only in the portion of tissue in contact with the perfusate fluid in the peritoneal cavity, and was not detectable in the deeper layers. The method cannot determine the absolute drug concentration and highlights only PTX ion signal presence over the background noise. Enlargements, shown in the insets, indicated that in patients A and B, PTX penetrated 0.54 and 0.41 mm in peritoneal tissue, and in patient C for 0.56 mm. The depth of penetration was deduced from the side of a square region of interest whose area was drawn and calculated using Tissue View software vs. 1.1 for the portion of tissue reached by the drug.
Discussion
In this study, intraperitoneal CDDP plus PTX combined with hyperthermia gave relative high levels of drug in the peritoneal cavity, in contact with tumour micrometastasis, compared with lower circulating plasma levels, consistently with literature (de Bree et al, 2008; Cashin et al, 2013). This pharmacokinetic profile is advantageous, achieving maximal antineoplastic effect against micrometastatic deposits in the peritoneal cavity, with minimal systemic toxicity. The levels of PTX and CDDP in peritoneal tissue, measured together for the first time in this study, were comparable with the concentrations in perfusate, suggesting that the drugs are efficiently taken up from the perfusate by peritoneal tissue, with minimal passage in the systemic circulation. In fact, the plasma levels of both drugs were lower than the toxic ones. Neutropenia, the dose-limiting toxicity of PTX, and neuropathy are related to PTX plasma concentrations >0.05 μmol l−1 lasting >10 hours (Wiernik et al, 1987; Mielke et al, 2006), which never happened in our patients. Similarly nephrotoxicity caused by CDDP can be avoided by keeping the plasma Cmax of the drug under 2 μg ml−1, like in our patients (Nagai et al, 1996). Alternatively, we could act by decreasing the duration of perfusion as pointed out by Cashin et al in 2013. The pharmacokinetics of CDDP studied by HPLC in fact demonstrates that the absorption of active CDDP is very rapid and probably not influenced by lowering the time of perfusion to 60 min. On the other hand, reducing the infusion time would not be advantageous for PTX, as at least in vitro the exposure time seems to be crucial for the cytotoxic effect of this drug.
Although the present study was performed on a limited number of patients, some of which were previously treated, and therefore it is difficult to draw conclusions on the toxicity, nevertheless it appears that the morbidity was quite significant and a high rate of hematological toxicity was observed as previously reported in other studies (Coccolini et al, 2013b). The toxicity seems manly due to the aggressive surgical procedure rather than the drug exposure that was relatively low, presumably under the toxicity threshold. The broad heterogeneity in the CDDP dosages in different studies, not correlated to different complication rates, further suggesting that the complications are related to the surgical procedure and not to CDDP treatment (Coccolini et al, 2013a).
The results of the present study are in keeping with previous reports on intraperitoneal use of PTX and give new information on the high drug concentration reached in peritoneal tissue. However, the penetration of PTX highlighted by MALDI IMS for the first time, is very limited, averaging 0.5 mm, less than that of CDDP, that is, 1–3 mm into tumour tissue assessed by other studies (Kerr and Kaye, 1987; Los et al, 1989; Kamei et al, 2011). These data support the view that HIPEC should be used only after complete CRS (no residual macroscopic disease or tumour deposits <2.5 mm).
The lack of satisfactory outcome for PC of different origin treated conventionally with surgery is due to the postsurgical microscopic persistence of the tumour, even after apparent radical macroscopic eradication of the tumour is achieved. The relapses indicate that post-surgical chemotherapy cannot kill all cancer cells nested in the peritoneal cavity. We do not know the level of resistance of those cells that will form the relapsing tumour mass, but as in the majority of resistant cell lines, high drug concentrations overcome the resistance, HIPEC could conceivably reduce the risk of relapse caused by micrometastatic lesions, also considering the potentiation of the drug’s effect by concomitant hyperthermia (Witkamp et al, 2001).
In conclusion, HIPEC with concomitant CDDP and PTX after CRS is feasible, safe and offers valuable advantages in terms of pharmacokinetic profile, despite the short treatment duration. Remarkably, in peritoneal tissue, the drugs reached concentrations several times higher than systemic ones, with only limited penetration in the deeper layer of healthy tissue. Larger studies are now needed to confirm its efficacy in patients with microscopic postsurgical residual tumours in the peritoneal cavity.
Change history
20 January 2015
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Ansaloni L, Agnoletti V, Amadori A, Catena F, Cavaliere D, Coccolini F, De Iaco P, Di Battista M, Framarini M, Gazzotti F, Ghermandi C, Kopf B, Saponara M, Tauceri F, Vallicelli C, Verdecchia GM, Pinna AD (2012) Evaluation of extensive cytoreductive surgery and hyperthermic intraperitoneal chemotherapy (HIPEC) in patients with advanced epithelial ovarian cancer. Int J Gynecol Cancer 22: 778–785.
Baratti D, Kusamura S, Cabras AD, Deraco M (2012) Cytoreductive surgery with selective versus complete parietal peritonectomy followed by hyperthermic intraperitoneal chemotherapy in patients with diffuse malignant peritoneal mesothelioma: a controlled study. Ann Surg Oncol 19: 1416–1424.
Canta A, Chiorazzi A, Carozzi V, Meregalli C, Oggioni N, Sala B, Crippa L, Avezza F, Forestieri D, Rotella G, Zucchetti M, Cavaletti G (2011) In vivo comparative study of the cytotoxicity of a liposomal formulation of cisplatin (lipoplatin). Cancer Chemother Pharmacol 68: 1001–1008.
Cashin PH, Ehrsson H, Wallin I, Nygren P, Mahteme H (2013) Pharmacokinetics of cisplatin during hyperthermic intraperitoneal treatment of peritoneal carcinomatosis. Eur J Clin Pharmacol 69: 533–540.
Cashin PH, Graf W, Nygren P, Mahteme H (2012) Intraoperative hyperthermic versus postoperative normothermic intraperitoneal chemotherapy for colonic peritoneal carcinomatosis: a case-control study. Ann Oncol 23: 647–652.
Cesca M, Frapolli R, Berndt A, Scarlato V, Richter P, Kosmehl H, D'Incalci M, Ryan AJ, Giavazzi R (2009) The effects of vandetanib on paclitaxel tumor distribution and antitumor activity in a xenograft model of human ovarian carcinoma. Neoplasia 11: 1155–1164.
Cho HK, Lush RM, Bartlett DL, Alexander HR, Wu PC, Libutti SK, Lee KB, Venzon DJ, Bauer KS, Reed E, Figg WD (1999) Pharmacokinetics of cisplatin administered by continuous hyperthermic peritoneal perfusion (CHPP) to patients with peritoneal carcinomatosis. J Clin Pharmacol 39: 394–401.
Chua TC, Liauw W, Morris DL (2012) Early recurrence of pseudomyxoma peritonei following treatment failure of cytoreductive surgery and perioperative intraperitoneal chemotherapy is indicative of a poor survival outcome. Int J Colorectal Dis 27: 381–389.
Coccolini F, Ansaloni L, Corbella D, Lotti M, Glehen O (2013a) Criticalities in randomized controlled trials on HIPEC for ovarian cancer. World J Obstet Gynecol 2: 124–128.
Coccolini F, Cotte E, Glehen O, Lotti M, Poiasina E, Catena F, Yonemura Y, Ansaloni L (2014) Intraperitoneal chemotherapy in advanced gastric cancer. Meta-analysis of randomized trials. Eur J Surg Oncol 40: 12–26.
Coccolini F, Gheza F, Lotti M, Virzi S, Iusco D, Ghermandi C, Melotti R, Baiocchi G, Giulini SM, Ansaloni L, Catena F (2013b) Peritoneal carcinomatosis. World J Gastroenterol 19: 6979–6994.
de Bree E, Rosing H, Filis D, Romanos J, Melisssourgaki M, Daskalakis M, Pilatou M, Sanidas E, Taflampas P, Kalbakis K, Beijnen JH, Tsiftsis DD (2008) Cytoreductive surgery and intraoperative hyperthermic intraperitoneal chemotherapy with paclitaxel: a clinical and pharmacokinetic study. Ann Surg Oncol 15: 1183–1192.
Elias D, Benizri E, Di Pietrantonio D, Menegon P, Malka D, Raynard B (2007) Comparison of two kinds of intraperitoneal chemotherapy following complete cytoreductive surgery of colorectal peritoneal carcinomatosis. Ann Surg Oncol 14: 509–514.
Fruscio R, Lissoni AA, Frapolli R, Corso S, Mangioni C, D'Incalci M, Zucchetti M (2006) Clindamycin-paclitaxel pharmacokinetic interaction in ovarian cancer patients. Cancer Chemother Pharmacol 58: 319–325.
Gonzalez-Moreno S, Kusamura S, Baratti D, Deraco M (2008) Postoperative residual disease evaluation in the locoregional treatment of peritoneal surface malignancy. J Surg Oncol 98: 237–241.
Huang SK, Stauffer PR, Hong K, Guo JW, Phillips TL, Huang A, Papahadjopoulos D (1994) Liposomes and hyperthermia in mice: increased tumor uptake and therapeutic efficacy of doxorubicin in sterically stabilized liposomes. Cancer Res 54: 2186–2191.
Kamei T, Kitayama J, Yamaguchi H, Soma D, Emoto S, Konno T, Ishihara K, Ishigami H, Kaisaki S, Nagawa H (2011) Spatial distribution of intraperitoneally administrated paclitaxel nanoparticles solubilized with poly (2-methacryloxyethyl phosphorylcholine-co n-butyl methacrylate) in peritoneal metastatic nodules. Cancer Sci 102: 200–205.
Kerr DJ, Kaye SB (1987) Aspects of cytotoxic drug penetration, with particular reference to anthracyclines. Cancer Chemother Pharmacol 19: 1–5.
Los G, Mutsaers PH, van der Vijgh WJ, Baldew GS, de Graaf PW, McVie JG (1989) Direct diffusion of cis-diamminedichloroplatinum(II) in intraperitoneal rat tumors after intraperitoneal chemotherapy: a comparison with systemic chemotherapy. Cancer Res 49: 3380–3384.
Los G, Verdegaal EM, Mutsaers PH, McVie JG (1991) Penetration of carboplatin and cisplatin into rat peritoneal tumor nodules after intraperitoneal chemotherapy. Cancer Chemother Pharmacol 28: 159–165.
Mielke S, Sparreboom A, Mross K (2006) Peripheral neuropathy: a persisting challenge in paclitaxel-based regimes. Eur J Cancer 42: 24–30.
Morosi L, Spinelli P, Zucchetti M, Pretto F, Carra A, D'Incalci M, Giavazzi R, Davoli E (2013) Determination of paclitaxel distribution in solid tumors by nano-particle assisted laser desorption ionization mass spectrometry imaging. PLoS One 8: e72532.
Nagai N, Kinoshita M, Ogata H, Tsujino D, Wada Y, Someya K, Ohno T, Masuhara K, Tanaka Y, Kato K, Nagai H, Yokoyama A, Kurita Y (1996) Relationship between pharmacokinetics of unchanged cisplatin and nephrotoxicity after intravenous infusions of cisplatin to cancer patients. Cancer Chemother Pharmacol 39: 131–137.
Royer B, Guardiola E, Polycarpe E, Hoizey G, Delroeux D, Combe M, Chaigneau L, Samain E, Chauffert B, Heyd B, Kantelip JP, Pivot X (2005) Serum and intraperitoneal pharmacokinetics of cisplatin within intraoperative intraperitoneal chemotherapy: influence of protein binding. Anticancer Drugs 16: 1009–1016.
Sugarbaker PH (2009) Cytoreductive surgery and perioperative intraperitoneal chemotherapy for the treatment of advanced primary and recurrent ovarian cancer. Curr Opin Obstet Gynecol 21: 15–24.
Uboldi S, Bernasconi S, Romano M, Marchini S, Fuso Nerini I, Damia G, Ganzinelli M, Marangon E, Sala F, Clivio L, Chiorino G, Di Giandomenico S, Rocchi M, Capozzi O, Margison GsP, Watson AJ, Caccuri AM, Pastore A, Fossati A, Mantovani R, Grosso F, Tercero JC, Erba E, D'Incalci M (2012) Characterization of a new trabectedin-resistant myxoid liposarcoma cell line that shows collateral sensitivity to methylating agents. Int J Cancer 131: 59–69.
Urano M, Kuroda M, Nishimura Y (1999) For the clinical application of thermochemotherapy given at mild temperatures. Int J Hyperthermia 15: 79–107.
Van der Speeten K, Stuart OA, Sugarbaker PH (2012) Pharmacology of perioperative intraperitoneal and intravenous chemotherapy in patients with peritoneal surface malignancy. Surg Oncol Clin N Am 21: 577–597.
Verwaal VJ, Bruin S, Boot H, van Slooten G, van Tinteren H (2008) 8-year follow-up of randomized trial: cytoreduction and hyperthermic intraperitoneal chemotherapy versus systemic chemotherapy in patients with peritoneal carcinomatosis of colorectal cancer. Ann Surg Oncol 15: 2426–2432.
Wang Y, Moss J, Thisted R (1992) Predictors of body surface area. J Clin Anesth 4: 4–10.
Wiernik PH, Schwartz EL, Strauman JJ, Dutcher JP, Lipton RB, Paietta E (1987) Phase I clinical and pharmacokinetic study of taxol. Cancer Res 47: 2486–2493.
Witkamp AJ, de Bree E, Van Goethem R, Zoetmulder FA (2001) Rationale and techniques of intra-operative hyperthermic intraperitoneal chemotherapy. Cancer Treat Rev 27: 365–374.
Yang XJ, Huang CQ, Suo T, Mei LJ, Yang GL, Cheng FL, Zhou YF, Xiong B, Yonemura Y, Li Y (2011) Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy improves survival of patients with peritoneal carcinomatosis from gastric cancer: final results of a phase III randomized clinical trial. Ann Surg Oncol 18: 1575–1581.
Zivanovic O, Abramian A, Kullmann M, Fuhrmann C, Coch C, Hoeller T, Ruehs H, Keyver-Paik MD, Rudlowski C, Weber S, Kiefer N, Poelcher ML, Thiesler T, Rostamzadeh B, Mallmann M, Schaefer N, Permantier M, Latten S, Kalff J, Thomale J, Jaehde U, Kuhn WC (2014) HIPEC ROC I: A phase i study of cisplatin administered as hyperthermic intraoperative intraperitoneal chemoperfusion followed by postoperative intravenous platinum-based chemotherapy in patients with platinum-sensitive recurrent epithelial ovarian cancer. Int J Cancer 136: 699–708.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Ansaloni, L., Coccolini, F., Morosi, L. et al. Pharmacokinetics of concomitant cisplatin and paclitaxel administered by hyperthermic intraperitoneal chemotherapy to patients with peritoneal carcinomatosis from epithelial ovarian cancer. Br J Cancer 112, 306–312 (2015). https://doi.org/10.1038/bjc.2014.602
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2014.602
Keywords
This article is cited by
-
Influence of hyperthermic intraperitoneal chemotherapy on renal blood perfusion
Langenbeck's Archives of Surgery (2023)
-
Dense hyperthermic intraperitoneal chemotherapy with cisplatin in patients with stage III serous epithelial ovarian cancer: a retrospective study
BMC Cancer (2021)
-
Calculating the dose of cisplatin that is actually utilized in hyperthermic intraperitoneal chemotherapy among ovarian cancer patients
Journal of Ovarian Research (2021)
-
Cytoreductive surgery with hyperthermic intraperitoneal chemotherapy for endometrial cancer-derived peritoneal metastases: a systematic review
Clinical & Experimental Metastasis (2019)
-
An innovative immunotherapeutic strategy for ovarian cancer: CLEC10A and glycomimetic peptides
Journal for ImmunoTherapy of Cancer (2018)