Abstract
Background:
There is increasing evidence that the presence of an ongoing systemic inflammatory response is a stage-independent predictor of poor outcome in patients with cancer. The aim of this study was to investigate whether an inflammation-based prognostic score, the prognostic nutritional index (PNI), is associated with overall survival (OS) in patients with hepatocellular carcinoma (HCC).
Methods:
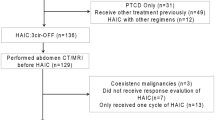
All patients with a new diagnosis of HCC presenting to the Medical Oncology Department, Hammersmith Hospital between 1993 and 2011 (n=112) were included. Demographic and clinical data were collected. Patients in whom the combined albumin (g l−1) × total lymphocyte count × 109 l−1 was ⩾45, at presentation, were allocated a PNI score of 0. Patients in whom this total score was <45 were allocated a score of 1. Univariate and multivariate analyses were performed to identify clinicopathological variables associated with OS. Independent predictors of survival identified on multivariate analysis were validated in an independent, stage-matched cohort of 68 patients.
Results:
Univariate analyses showed that PNI (P=0.003), intrahepatic spread (P<0.001), the presence of extrahepatic disease (P=0.006), portal vein thrombosis (P=0.02), tumour multifocality (P=0.003), alfa-fetoprotein >400 ng ml−1 (P<0.001) and Barcelona Clinic Liver Cancer score (P<0.01) were all predictors of OS in the training set. Multivariate analysis revealed the PNI (P=0.05), presence of extrahepatic disease (P<0.001) and degree of intrahepatic spread (P<0.001) as independent predictors of worse OS in this population. The PNI retained independent prognostic value in the validation set (P<0.001).
Conclusion:
The presence of a systemic inflammatory response, as measured by the PNI, is an independent and externally validated predictor of poor OS in patients with HCC.
Similar content being viewed by others
Main
Hepatocellular carcinoma (HCC) is the sixth most common neoplasm, and the third most lethal accounting for more than 600 000 deaths per year worldwide (Parkin et al, 2005). In countries with active surveillance programs, HCC is diagnosed at an early stage in 30 to 40% of patients and is amenable to potentially curative treatments, such as surgical resection and liver transplantation. However, for the majority of patients palliation is the only treatment option, owing to the fact that most tumors are diagnosed at an advanced stage. Sorafenib is the standard of care in patients with advanced disease, but has limited efficacy, with only a 3-month improvement in overall survival (OS) (Llovet et al, 2008). There is a need therefore to further delineate prognostic determinants of survival in order to better stratify those patients likely to benefit from treatment in order to avoid unnecessary toxicity and morbidity.
The pathogenesis of HCC is based on inflammation such that the chronically inflamed liver parenchyma represents a preneoplastic environment in which HCC can arise as a result of the exposure to a plethora of pro-inflammatory stimuli such as infection by hepatotropic viruses, iron or copper accumulation or ethanol consumption (Berasain et al, 2009). Unlike other malignancies, survival in HCC patients is peculiarly influenced by the underlying liver function along with the extent of spread of the primary tumour (Bruix et al, 2001). The most commonly used prognostic algorithms variably incorporate predictors reflecting liver functional reserve, performance status as well as the tumour stage, however despite there being seven different prognostic scores, there is little consensus in the literature as to the most reliable (Camma and Cabibbo, 2009). The two most commonly used scores are the Barcelona Clinic Liver Cancer (BCLC) (Llovet et al, 1999) and Cancer of the Liver Italian Program (CLIP) scores (Investigators CLIP, 1998). The BCLC score is an optimally designed treatment algorithm but recent evidence has shown its limited predictive value in estimating survival in patients with advanced HCC (Huitzil-Melendez et al, 2010). Despite having shown good predictive capacity across all the stages of HCC (Hsu et al, 2010), the CLIP score subcategorizes patients in seven prognostic strata, therefore reducing its applicability to routine clinical practice. There is a need therefore for a reliable, easy to use prognostic score.
There is increasing evidence showing that the presence of a systemic inflammatory response, as indicated by an elevated circulating C-reactive protein (CRP) concentration, is associated with poor survival in patients with malignancy, including HCC (Hashimoto et al, 2005; Nagaoka et al, 2007). Furthermore, the presence of an inflammatory response is proposed to be pathogenic in the development of cancer-associated malnutrition (Argiles et al, 2003a, 2003b). Nutritional impairment in turn is correlated with poor performance status, shorter survival, and increased mortality in patients with cancer (Andreyev et al, 1998; Dewys et al, 1980; Rey-Ferro et al, 1997; Jagoe et al, 2001). This is of particular concern in patients with HCC, given the concomitant underlying illnesses and possible impaired nutritional status secondary to cirrhosis (Meng et al, 2010). The prognostic nutritional index (PNI) has been shown to be a prognostic marker in a number of gastrointestinal malignancies (Nozoe et al, 2002, 2010; Kanda et al, 2011), and, more recently, in a large study by Proctor et al (2011), the PNI was found to predict prognosis in malignancy regardless of the site of origin. The aim of the present study is to examine the relationship between the PNI and survival in patients with HCC.
Patients and methods
We conducted a retrospective analysis of all the patients with a diagnosis of HCC presenting to the Medical Oncology Department, Hammersmith Hospital between 1993 and 2011, excluding those cases with a positive history of inflammatory disease or active concomitant infection. All the patients included satisfied the diagnosis of HCC made according to radiological or histological criteria as recommended by the American Association for the Study of the Liver guidelines (Bruix and Sherman, 2005). Clinical variables, including demographic data, complete blood picture, albumin, alpha-fetoprotein (AFP), staging of the tumour, including the number of focal hepatic lesions, maximum diameter detected during contrast enhancement phase and degree of intra-hepatic spread, and Child–Turcotte–Pugh (CTP) class were collected. The presence of liver cirrhosis was diagnosed using clinical and radiological criteria (computerised tomography scan) in all patients. A proportion of the cirrhotic subjects included in this study had histological evidence of liver cirrhosis (45%). Overall (cancer-specific) survival was computed from the time of referral to our unit.
The PNI was calculated as described previously (Nozoe et al, 2010) where combined albumin (g l−1) × total lymphocyte count × 109 l−1 ⩾45, at presentation, were allocated a PNI score of 0. Patients in whom this total was <45 were allocated a PNI score of 1, where a PNI of 1 is indicative of severe nutritional impairment and PNI of 0 is normal.
The significance of the tested prognostic models was externally validated using an independent set of consecutive, stage-matched patients presenting to the St Mary's and Charing Cross Hospitals (n=68).
By using OS as a measure of outcome we further evaluated the independent prognostic power of the PNI in comparison with commonly used prognostic scores, including the CLIP score and the BCLC staging system on the complete set of patients (n=180). Both CLIP and BCLC prognostic models were calculated as previously described (Investigators CLIP, 1998; Llovet et al, 1999).
Each score was further tested for homogeneity, discrimination and monotonicity in order to estimate the accuracy of outcome prediction as recommended in previously published studies (Ueno et al, 2001). The study was approved by the local Research Ethics Committee.
Statistical analysis
Survival (cancer-specific) analysis was carried out using the Cox proportional hazard model. Multivariate survival analysis was performed using a stepwise backward procedure to derive a final model of the variables that had a significant independent relationship with survival. To remove a variable from the model, the corresponding P-value had to be >0.10. To avoid colinearity bias, the independent prognostic power of the PNI was preliminarily tested on a first multivariate model that included the individual variables composing the BCLC and CLIP score.
The discriminative ability of each prognostic score was tested using rms packages of Dr Frank Harrell to identify a subset of predictors by backward elimination (Harrell, 2001). Where we assessed the predictive ability of a Cox proportional hazards model, we compared the actual survival outcomes of usable pairs of patients with the values of their estimated prognostic indices from the Cox model. Where the assessment of prediction of multiple biomarkers was performed, the C-index was adjusted within the rms package for the over-optimism produced by modeling and assessment being done on the same data via comparison with 150 bootstrap samples. The monotonicity of each score was assessed with the linear trend χ2 test, whereas the homogeneity of prognostic prediction across categories was tested using the likelihood ratio test as previously described (Ueno et al, 2001). Pearson's χ2 test was used to test the effects of PNI on clinicopathological factors. All analyses except for C-index were performed using SPSS software version 19 (SPSS Inc., Chicago, IL, USA).
Results
The training set consisted of 112 patients whose baseline clinicopathological characteristics are shown in Table 1. The majority of patients had compensated liver function (Child–Turcotte–Pugh Class A, 65%), had underlying cirrhosis (63%), and were staged as being intermediate (56/112, 50%) or advanced (38/112, 34%) according to the BCLC algorithm. The median age of the patients at study baseline was 65 years (range 20–83). The majority of patients had received at least one line of active treatment (68%), including locoregional (52%) or systemic treatments (21%). All remaining patients were offered best supportive care (32%). At presentation, albumin and total lymphocyte count was measured in all 112 and 105 patients, respectively. Median serum albumin was 32 mg dl−1 (range 14–48 mg dl−1) and median total lymphocyte count was 1.6 × 109 l−1 (0.4–4.4 × 109 l−1). Sixty-one patients (55%) had an abnormal PNI.
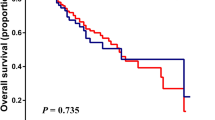
At the time of analysis 81 (72%) patients had died and overall median survival was 6.4 months (range 1–88 months). On univariate analysis, PNI (P<0.05, Figure 1), presence of extrahepatic disease (P=0.05), portal vein thrombosis (P<0.05), AFP >400 (P<0.001), degree of intrahepatic spread (<0.001) and BCLC stage (P<0.01) were significant predictors of cancer-specific survival (Table 2). On multivariate analysis, PNI (P<0.05), presence of metastases (P=0.01) and degree of intrahepatic spread (P<0.001) remained significant independent predictors of cancer specific survival. The median survival in patients with a PNI of 0 was 16 compared with 6 months in patients with a PNI of 1 (hazard ratio (HR) 2.02, 95% confidence interval (CI) 1.26–3.23, P=0.03).
A significant association was observed between PNI 1 and raised AFP (47%, 20 of 43) (P<0.05). Patients with PNI 1 were also more likely to have portal vein thrombosis P<0.05) and worse CTP class (P<0.001) (Table 1). No other associations were observed.
An independent set of 68 consecutive patients was used to statistically validate the prognostic model identified in the training set. These cases were matching by stage to those in the training set, with the degree of intrahepatic (P=0.94) and extrahepatic spread (P=0.25), the number of tumours (P=0.29) being homogeneously distributed across the groups. Median OS in the validation set was 5.4 months and not significantly different compared with that of the training set (P=0.23). In the validation set, the PNI (HR 4.54 95% CI 2.04–10.1, P<0.001) together with the presence of extrahepatic disease (HR 3.86 95% CI 1.61–9.22, P=0.02) and the extent of intrahepatic spread (HR 1.83 95% CI 1.11–2.99, P=0.01) were univariate predictors of survival. The PNI (HR 5.11 95% CI 2.27–11.49, P<0.001) and the presence of extrahepatic spread (HR 4.38 95% CI 1.69–11.36, P=0.002) were confirmed as independent predictors of OS.
The independent prognostic ability of the PNI, BCLC and CLIP score was then assessed using a multivariate Cox regression model in a combined assessment of all patients (n=180). This analysis identified the PNI and CLIP score as the strongest independent predictors of survival (Table 3). As shown in Table 4, the accuracy of the PNI is superior to that of the CLIP and BCLC scores in terms of monotonicity and homogeneity of prognostic prediction, although C-index analysis revealed the CLIP score to have superior discriminative ability compared with the other scores.
Discussion
In the present study, a simple inflammation-based prognostic score (PNI) was shown to be an independent predictor of survival in patients with HCC. This measure of inflammation is based on standard laboratory measurements of total lymphocyte count and albumin, which are routinely measured in the clinical setting. These results are consistent with a number of previous studies investigating the prognostic role of hypoalbuminaemia and lymphocytopenia in both gastro-oesophageal and pancreatic cancer (Nozoe et al, 2002, 2010; Kanda et al, 2011), as well as liver cirrhosis (Carvalho and Parise, 2006).
The PNI was initially designed to assess the immunological and nutritional aspects of patients undergoing surgery of the gastrointesintal tract, predominantly as an indicator of the nutritional status of any given patient (Nozoe et al, 2002, 2010; Kanda et al, 2011). Albumin is a widely used indicator of nutrition and has been shown to correlate with post-operative complications (Fujiwara et al, 2010; Ellis et al, 2011; Lai et al, 2011). However there is increasing evidence that the presence of cancer cachexia, partly reflected by a reduction in albumin, is driven by a sustained inflammatory response, either from the tumour itself or as a host reaction (Esper and Harb, 2005). Furthermore, a number of studies have illustrated that the presence of inflammation is reflected in routine haematology with a number of inflammation-based prognostic scores validated in patients with malignancy (McMillan, 2009). In the context of HCC, the neutrophil to lymphocyte ratio (NLR), a simple biomarker derived from the circulating differential white blood cell count, has been associated with reduced survival (Gomez et al, 2008; Halazun et al, 2009; Chen et al, 2011). Another inflammatory index, the modified Glasgow Prognostic Score, based on CRP and albumin has been shown to predict OS in a large cohort of patients (Ishizuka et al, 2011). Therefore, although initially thought of as purely a reflection of the nutritional status of a patient, it is likely, given its prognostic association, that the PNI is a reflection of systemic inflammation.
Previous studies have investigated a number of possible prognostic factors in HCC. In particular the adverse effect of portal vein thrombosis, extra-hepatic spread, tumour multifocality and elevated AFP on patients OS has emerged from previously published studies (El-Serag et al, 2008). In the present study we found that PNI was superior to the presence of PVT and AFP in predicting OS of a cohort of patients with intermediate-advanced HCC, which is of greater consequence in the management of this patient population, as treatment decisions are often based on the presence of PVT. Consistent with previous studies we found that on multivariate analysis the presence of metastatic disease and intrahepatic spread remained as independent predictors of OS. We noted that PNI correlated significantly with raised AFP, liver functional reserve and the presence of portal vein thrombosis suggesting that a high risk PNI correlates with a more aggressive disease phenotype. Interestingly, the independent prognostic value of the PNI was strengthened by a process of cross-validation, which confirmed the PNI as a stage independent predictor of OS in HCC.
Lastly, our comparative assessment of the PNI with established prognostic systems in HCC confirmed the robustness of the prognostic information conveyed by the PNI, which ranked first in terms of prognostic monotonicity and homogeneity and held a discriminative capacity comparable to that of more complex prognostic systems such as the BCLC. Although the generalizability of our results is limited by the retrospective nature of this clinical study, such finding is of greater consequence in the clinical management of HCC, where there is little consensus in the literature on the optimum staging system, many of which are cumbersome and used only in the clinical trials setting (Camma and Cabibbo, 2009). The population studied consisted of patients presenting to medical oncology outpatient department and thereby consisted predominantly of intermediate and advanced-stage disease. In future studies it would be important to include patients presenting to both hepatobiliary surgeons and hepatologists for routine screening for HCC in order to validate the PNI across all stages of HCC. Moreover, it would be important to compare the utility of PNI with these other staging systems in an independent validation cohort, ideally collected in a prospective fashion.
This step is warranted before the PNI can be used with confidence to estimate survival in individual patients. Furthermore, it would be of interest to correlate PNI with possible pro-inflammatory cytokines and more robust measures of cachexia such as the Patient-Generated Subjective Global Assessment (PGSGA) (Read et al, 2005).
This has been previously explored in a small study by Read and colleagues in patients with metastatic colorectal cancer that suggested that there is a correlation with CRP and PGSGA (Read et al, 2006). Interestingly a significant association between deranged nutrition scores and inflammatory markers such as low albumin and elevated CRP has been documented in HCC (Tsai et al, 2011), suggesting that simple inflammatory markers such as the PNI could be implemented in the routine nutritional assessment.
The mechanism by which systemic inflammation may impact on survival is not completely understood. A number of studies appear to reinforce the biological plausibility behind systemic inflammation and the prognosis of HCC. Lymphopenia is a renown adverse prognostic factor in solid tumours (Ray-Coquard et al, 2009) and convincing evidence supports the concept that the impairment of lymphocyte mediated antitumour response is an immunological determinant of patients prognosis in HCC (Yang et al, 2010). Moreover, it is well understood that inflammatory pathways can be redirected into a tumour-promoting path by the peritumoural stroma through the activation of innate immunity in HCC (Kuang et al, 2011).
This is particularly true in the context of HCC, where cytokines such as interleukin-6 (IL-6) have been identified as candidate molecular risk factors for HCC acting on chronically inflamed hepatocytes (Naugler et al, 2007; Prieto, 2008; Falleti et al, 2009). In addition, the production of circulating CRP largely upon IL-6 (Kinoshita et al, 1999; McKeown et al, 2004). Interleukin-6 has been shown to increase the anti-apoptotic and oncogenic potential of tumour cells, as well as inducing drug resistance in vitro (Jee et al, 2001; Yusuf et al, 2003). Furthermore, it has been proposed that elevated CRP identifies those patients with T-lymphocyte impairment, which is associated with poor outcome in malignancy (Canna et al, 2005). On the other hand, sustained inflammation may reflect a pro-angiogenic environment, as circulating concentrations of vascular endothelial growth factor are directly associated with CRP, allowing unrestrained tumour growth and dissemination (Kemik et al, 2010; Reynes et al, 2011).
Hepatic albumin biosynthesis is downregulated by pro-inflammatory stimuli as part of a negative acute phase reaction in patients with malignancy (Steel and Whitehead, 1994). However, impaired synthetic functions accompanying end-stage liver disease needs to be considered as an additional determinant of reduced serum albumin that may have contributed to the results reported. Although previous reports show the independent prognostic value of hypoalbuminaemia in HCC (Hao et al, 2009; Nouso et al, 2010), our data are not consistent with this finding suggesting that the reduced survival observed in patients with a PNI of 1 was not solely a reflection of impaired liver function.
More recently, the presence of a systemic inflammatory response has been shown to impair the activity of cytochrome 3A (CYP3A4) in patients with advanced cancer patients (Rivory et al, 2002; Charles et al, 2006). As CYP3A4 is the principal drug-metabolising enzyme for over 60% of all prescribed medications, including sorafenib, changes in the activity of CYP3A4 may result in impaired drug response or increased toxicity (Charles et al, 2006). It is further hypothesised that high protein catabolism, and stimulation of the acute phase response, may induce perturbations of the cellular response to chemotherapy-induced DNA damage in normal tissues and result in increased toxicity. Moreover, nutrition may alter the pharmacokinetics of many anticancer agents through altered protein binding and P450 activity (Murry et al, 1998; Rivory et al, 2002). Prognostic nutritional index therefore, may not only be a valuable tool in prognostication but may also be used to predict those patients at risk of developing toxicity. Dose adjustments before the initiation of treatment in this patient group may improve the tolerability of anticancer agents and help maintain dose intensity. However, this concept requires further evaluation in a prospectively designed trial.
Irrespective of the mechanisms involved, the results of the present study suggest that the presence of a systemic inflammatory response, as indicated by PNI, is a useful tool in the assessment of survival in patients with HCC. As described, the PNI could function as a surrogate marker for the complex interplay between inflammatory pathways, angiogenesis and tumour progression that are known to have an impact on patient survival. PNI is simple to construct from laboratory measures that are routinely assessed in patients before treatment. Prognostic nutritional index therefore should be further evaluated not only as a prognostic marker in patients with HCC at diagnosis, and in the stratification of patients entering clinical trials.
Change history
23 January 2013
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Andreyev HJ, Norman AR, Oates J, Cunningham D (1998) Why do patients with weight loss have a worse outcome when undergoing chemotherapy for gastrointestinal malignancies? Eur J Cancer 34 (4): 503–509
Argiles JM, Busquets S, Lopez-Soriano FJ (2003a) Cytokines in the pathogenesis of cancer cachexia. Curr Opin Clin Nutr Metab Care 6 (4): 401–406
Argiles JM, Moore-Carrasco R, Fuster G, Busquets S, Lopez-Soriano FJ (2003b) Cancer cachexia: the molecular mechanisms. Int J Biochem Cell Biol 35 (4): 405–409
Berasain C, Castillo J, Perugorria MJ, Latasa MU, Prieto J, Avila MA (2009) Inflammation and liver cancer: new molecular links. Ann NY Acad Sci 1155: 206–221
Bruix J, Sherman M (2005) Management of hepatocellular carcinoma. Hepatology 42 (5): 1208–1236
Bruix J, Sherman M, Llovet JM, Beaugrand M, Lencioni R, Burroughs AK, Christensen E, Pagliaro L, Colombo M, Rodés J (2001) Clinical Management of Hepatocellular Carcinoma. Conclusions of the Barcelona-2000 EASL Conference. J Hepatol 35 (3): 421–430
Camma C, Cabibbo G (2009) Prognostic scores for hepatocellular carcinoma: none is the winner. Liver Int 29 (4): 478–480
Canna K, McArdle PA, McMillan DC, McNicol AM, Smith GW, McKee RF, McArdle CS (2005) The relationship between tumour T-lymphocyte infiltration, the systemic inflammatory response and survival in patients undergoing curative resection for colorectal cancer. Br J Cancer 92 (4): 651–654
Carvalho L, Parise ER (2006) Evaluation of nutritional status of nonhospitalized patients with liver cirrhosis. Arquivos de Gastroenterologia 43 (4): 269–274
Charles KA, Rivory LP, Brown SL, Liddle C, Clarke SJ, Robertson GR (2006) Transcriptional repression of hepatic cytochrome P450 3A4 gene in the presence of cancer. Clin Cancer Res Official J Am Assoc Cancer Res 12 (24): 7492–7497
Chen TM, Lin CC, Huang PT, Wen CF (2011) Neutrophil-to-lymphocyte ratio associated with mortality in early hepatocellular carcinoma patients after radiofrequency ablation. J Gastroenterol Hepatol 27 (3): 553–561
Dewys WD, Begg C, Lavin PT, Band PR, Bennett JM, Bertino JR, Cohen MH, Douglass Jr HO, Engstrom PF, Ezdinli EZ, Horton J, Johnson GJ, Moertel CG, Oken MM, Perlia C, Rosenbaum C, Silverstein MN, Skeel RT, Sponzo RW, Tormey DC (1980) Prognostic effect of weight loss prior to chemotherapy in cancer patients. Eastern Cooperative Oncology Group. Am J Med 69 (4): 491–497
Ellis MC, Cassera MA, Vetto JT, Orloff SL, Hansen PD, Billingsley KG (2011) Surgical treatment of intrahepatic cholangiocarcinoma: outcomes and predictive factors. HPB Official J Int Hepato Pancreato Biliary Assoc 13 (1): 59–63
El-Serag HB, Marrero JA, Rudolph L, Reddy KR (2008) Diagnosis and treatment of hepatocellular carcinoma. Gastroenterology 134 (6): 1752–1763
Esper DH, Harb WA (2005) The cancer cachexia syndrome: a review of metabolic and clinical manifestations. Nutr Clin Pract 20 (4): 369–376
Falleti E, Fabris C, Toniutto P, Fontanini E, Cussigh A, Bitetto D, Fumolo E, Fornasiere E, Bragagnini W, Pinato DJ, Minisini R, Pirisi M (2009) Interleukin-6 polymorphisms and gender: relationship with the occurrence of hepatocellular carcinoma in patients with end-stage liver disease. Oncology 77 (5): 304–313
Fujiwara Y, Shiba H, Furukawa K, Iida T, Haruki K, Gocho T, Wakiyama S, Hirohara S, Ishida Y, Misawa T, Ohashi T, Yanaga K (2010) Glasgow prognostic score is related to blood transfusion requirements and post-operative complications in hepatic resection for hepatocellular carcinoma. Anticancer Res 30 (12): 5129–5136
Gomez D, Farid S, Malik HZ, Young AL, Toogood GJ, Lodge JP, Prasad KR (2008) Preoperative neutrophil-to-lymphocyte ratio as a prognostic predictor after curative resection for hepatocellular carcinoma. World J Surg 32 (8): 1757–1762
Halazun KJ, Hardy MA, Rana AA, Woodland DCT, Luyten EJ, Mahadev S, Witkowski P, Siegel AB, Brown Jr RS, Emond JC (2009) Negative impact of neutrophil-lymphocyte ratio on outcome after liver transplantation for hepatocellular carcinoma. Ann Surg 250 (1): 141–151
Hao K, Luk JM, Lee NP, Mao M, Zhang C, Ferguson MD, Lamb J, Dai H, Ng IO, Sham PC, Poon RT (2009) Predicting prognosis in hepatocellular carcinoma after curative surgery with common clinicopathologic parameters. BMC Cancer 9: 389
Harrell FE (2001) Regression Modeling Strategies. Springer: New York
Hashimoto K, Ikeda Y, Korenaga D, Tanoue K, Hamatake M, Kawasaki K, Yamaoka T, Iwatani Y, Akazawa K, Takenaka K (2005) The impact of preoperative serum C-reactive protein on the prognosis of patients with hepatocellular carcinoma. Cancer 103 (9): 1856–1864
Hsu CY, Hsia CY, Huang YH, Su CW, Lin HC, Lee PC, Loong CC, Chiang JH, Huo TI, Lee SD (2010) Selecting an optimal staging system for hepatocellular carcinoma: comparison of 5 currently used prognostic models. Cancer 116 (12): 3006–3014
Huitzil-Melendez FD, Capanu M, O’Reilly EM, Duffy A, Gansukh B, Saltz LL, Abou-Alfa GK (2010) Advanced hepatocellular carcinoma: which staging systems best predict prognosis? J Clin Oncol 28 (17): 2889–2895
Investigators CLIP (1998) A new prognostic system for hepatocellular carcinoma: a retrospective study of 435 patients: the Cancer of the Liver Italian Program (CLIP) investigators. Hepatology 28 (3): 751–755
Ishizuka M, Kubota K, Kita J, Shimoda M, Kato M, Sawada T (2011) Impact of an inflammation-based prognostic system on patients undergoing surgery for hepatocellular carcinoma: a retrospective study of 398 Japanese patients. Am J Surg 203 (1): 101–106
Jagoe RT, Goodship TH, Gibson GJ (2001) Nutritional status of patients undergoing lung cancer operations. Ann Thorac Surg 71 (3): 929–935
Jee SH, Shen SC, Chiu HC, Tsai WL, Kuo ML (2001) Overexpression of interleukin-6 in human basal cell carcinoma cell lines increases anti-apoptotic activity and tumorigenic potency. Oncogene 20 (2): 198–208
Kanda M, Fujii T, Kodera Y, Nagai S, Takeda S, Nakao A (2011) Nutritional predictors of postoperative outcome in pancreatic cancer. Br J Surg 98 (2): 268–274
Kemik O, Sumer A, Kemik AS, Hasirci I, Purisa S, Dulger AC, Demiriz B, Tuzun S (2010) The relationship among acute-phase response proteins, cytokines and hormones in cachectic patients with colon cancer. World J Surg Oncol 8: 85
Kinoshita T, Ito H, Miki C (1999) Serum interleukin-6 level reflects the tumor proliferative activity in patients with colorectal carcinoma. Cancer 85 (12): 2526–2531
Kuang DM, Zhao Q, Wu Y, Peng C, Wang J, Xu Z, Yin XY, Zheng L (2011) Peritumoral neutrophils link inflammatory response to disease progression by fostering angiogenesis in hepatocellular carcinoma. J Hepatol 54 (5): 948–955
Lai CC, You JF, Yeh CY, Chen JS, Tang R, Wang JY, Chin CC (2011) Low preoperative serum albumin in colon cancer: a risk factor for poor outcome. Int J Colorectal Dis 26 (4): 473–481
Llovet JM, Bru C, Bruix J (1999) Prognosis of hepatocellular carcinoma: the BCLC staging classification. Semin Liver Dis 19 (3): 329–338
Llovet JM, Ricci S, Mazzaferro V, Hilgard P, Gane E, Blanc JF, de Oliveira AC, Santoro A, Raoul JL, Forner A, Schwartz M, Porta C, Zeuzem S, Bolondi L, Greten TF, Galle PR, Seitz JF, Borbath I, Haussinger D, Giannaris T, Shan M, Moscovici M, Voliotis D, Bruix J (2008) Sorafenib in advanced hepatocellular carcinoma. N Engl J Med 359 (4): 378–390
McKeown DJ, Brown DJ, Kelly A, Wallace AM, McMillan DC (2004) The relationship between circulating concentrations of C-reactive protein, inflammatory cytokines and cytokine receptors in patients with non-small-cell lung cancer. Br J Cancer 91 (12): 1993–1995
McMillan DC (2009) Systemic inflammation, nutritional status and survival in patients with cancer. Curr Opin Clin Nutr Metab Care 12 (3): 223–226
Meng QH, Yu HW, Li J, Wang JH, Ni MM, Feng YM, Jin Y, Hou W, Yu SQ, Wang X, Liu Y (2010) Inadequate nutritional intake and protein-energy malnutrition involved in acute and chronic viral hepatitis Chinese patients especially in cirrhosis patients. Hepatogastroenterology 57 (101): 845–851
Murry DJ, Riva L, Poplack DG (1998) Impact of nutrition on pharmacokinetics of anti-neoplastic agents. Int J Cancer Suppl 11: 48–51
Nagaoka S, Yoshida T, Akiyoshi J, Akiba J, Torimura T, Adachi H, Kurogi J, Tajiri N, Inoue K, Niizeki T, Koga H, Imaizumi T, Kojiro M, Sata M (2007) Serum C-reactive protein levels predict survival in hepatocellular carcinoma. Liver Int 27 (8): 1091–1097
Naugler WE, Sakurai T, Kim S, Maeda S, Kim K, Elsharkawy AM, Karin M (2007) Gender disparity in liver cancer due to sex differences in MyD88-dependent IL-6 production. Science 317 (5834): 121–124
Nouso K, Kobayashi Y, Nakamura S, Kobayashi S, Toshimori J, Kuwaki K, Hagihara H, Onishi H, Miyake Y, Ikeda F, Shiraha H, Takaki A, Iwasaki Y, Kobashi H, Yamamoto K (2010) Evolution of prognostic factors in hepatocellular carcinoma in Japan. Aliment Pharmacol Ther 31 (3): 407–414
Nozoe T, Kimura Y, Ishida M, Saeki H, Korenaga D, Sugimachi K (2002) Correlation of pre-operative nutritional condition with post-operative complications in surgical treatment for oesophageal carcinoma. Eur J Surg OncolJ Eur Soc Surg Oncol Br Assoc Surg Oncol 28 (4): 396–400
Nozoe T, Ninomiya M, Maeda T, Matsukuma A, Nakashima H, Ezaki T (2010) Prognostic nutritional index: a tool to predict the biological aggressiveness of gastric carcinoma. Surg Today 40 (5): 440–443
Parkin DM, Bray F, Ferlay J, Pisani P (2005) Global cancer statistics, 2002. CA Cancer J Clin 55 (2): 74–108
Prieto J (2008) Inflammation, HCC and sex: IL-6 in the centre of the triangle. J Hepatol 48 (2): 380–381
Proctor MJ, Morrison DS, Talwar D, Balmer SM, Fletcher CD, O’Reilly DS, Foulis AK, Horgan PG, McMillan DC (2011) A comparison of inflammation-based prognostic scores in patients with cancer. A Glasgow Inflammation Outcome Study. Eur J Cancer 47 (17): 2633–2641
Ray-Coquard I, Cropet C, Van Glabbeke M, Sebban C, Le Cesne A, Judson I, Tredan O, Verweij J, Biron P, Labidi I, Guastalla JP, Bachelot T, Perol D, Chabaud S, Hogendoorn PC, Cassier P, Dufresne A, Blay JY (2009) Lymphopenia as a prognostic factor for overall survival in advanced carcinomas, sarcomas, and lymphomas. Cancer Res 69 (13): 5383–5391
Read JA, Choy ST, Beale PJ, Clarke SJ (2006) Evaluation of nutritional and inflammatory status of advanced colorectal cancer patients and its correlation with survival. Nutr Cancer 55 (1): 78–85
Read JA, Crockett N, Volker DH, MacLennan P, Choy ST, Beale P, Clarke SJ (2005) Nutritional assessment in cancer: comparing the Mini-Nutritional Assessment (MNA) with the scored Patient-Generated Subjective Global Assessment (PGSGA). Nutr Cancer 53 (1): 51–56
Rey-Ferro M, Castano R, Orozco O, Serna A, Moreno A (1997) Nutritional and immunologic evaluation of patients with gastric cancer before and after surgery. Nutrition 13 (10): 878–881
Reynes G, Vila V, Martin M, Parada A, Fleitas T, Reganon E, Martinez-Sales V (2011) Circulating markers of angiogenesis, inflammation, and coagulation in patients with glioblastoma. J Neurooncol 102 (1): 35–41
Rivory LP, Slaviero KA, Clarke SJ (2002) Hepatic cytochrome P450 3A drug metabolism is reduced in cancer patients who have an acute-phase response. Br J Cancer 87 (3): 277–280
Steel DM, Whitehead AS (1994) The major acute phase reactants: C-reactive protein, serum amyloid P component and serum amyloid A protein. Immunol Today 15 (2): 81–88
Tsai AC, Hsu WC, Chan SC, Chang TL (2011) Usefulness of the mini nutritional assessment in predicting the nutritional status of patients with liver cancer in Taiwan. Nutr Cancer 63 (3): 334–341
Ueno S, Tanabe G, Sako K, Hiwaki T, Hokotate H, Fukukura Y, Baba Y, Imamura Y, Aikou T (2001) Discrimination value of the new western prognostic system (CLIP score) for hepatocellular carcinoma in 662 Japanese patients. Cancer of the Liver Italian Program. Hepatology 34 (3): 529–534
Yang ZQ, Yang ZY, Zhang LD, Ping B, Wang SG, Ma KS, Li XW, Dong JH (2010) Increased liver-infiltrating CD8+FoxP3+ regulatory T cells are associated with tumor stage in hepatocellular carcinoma patients. Hum Immunol 71 (12): 1180–1186
Yusuf RZ, Duan Z, Lamendola DE, Penson RT, Seiden MV (2003) Paclitaxel resistance: molecular mechanisms and pharmacologic manipulation. Curr Cancer Drug Targets 3 (1): 1–19
Acknowledgements
The authors would like to acknowledge the contribution of Ms Lynn Maslen for her helpful revision of the manuscript and Dr Harpreet Wasan for having supported this study. DJP has received support from the Fondazione De Agostini Grant for PhD studies.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Pinato, D., North, B. & Sharma, R. A novel, externally validated inflammation-based prognostic algorithm in hepatocellular carcinoma: the prognostic nutritional index (PNI). Br J Cancer 106, 1439–1445 (2012). https://doi.org/10.1038/bjc.2012.92
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2012.92
Keywords
This article is cited by
-
The prognostic value of the advanced lung cancer inflammation index in patients with gastrointestinal malignancy
BMC Cancer (2023)
-
Impact of Geriatric Nutritional Risk Index After Initial Hepatectomy for Hepatocellular Carcinoma: a Retrospective Cohort Study with the Hiroshima Surgical Study Group of Clinical Oncology (HiSCO)
Journal of Gastrointestinal Surgery (2023)
-
Laparoscopic liver resection is associated with less significant muscle loss than the conventional open approach
World Journal of Surgical Oncology (2022)
-
The monocyte to lymphocyte ratio not only at baseline but also at relapse predicts poor outcomes in patients with hepatocellular carcinoma receiving locoregional therapy
BMC Gastroenterology (2022)
-
Development of nomogram models of inflammatory markers based on clinical database to predict prognosis for hepatocellular carcinoma after surgical resection
BMC Cancer (2022)