Abstract
Background:
Despite neoadjuvant/adjuvant chemotherapy, women with resectable stage II/III breast cancer (BC) have high risk of recurrent disease. Recent data suggest that zoledronic acid (ZOL) therapy concurrent with adjuvant treatments may improve cancer-related outcomes in patients with BC.
Methods:
Disease-free survival (DFS; secondary end point) and overall survival (OS; tertiary end point) were evaluated in 119 women with stage II/III BC randomised to intravenous ZOL 4 mg every 3 weeks for 1 year or no ZOL (control) starting with the first chemotherapy cycle.
Results:
At 61.9 months’ median follow-up, there was no significant difference in recurrence or survival between study arms. However, time to recurrence or death (DFS) was significantly different between subgroups defined by oestrogen receptor (ER) status (interaction P=0.010 for DFS and 0.025 for OS). Hazard ratios (HRs) for disease recurrence and death were significantly less among patients with ER-negative (ER−) tumours who received ZOL vs no ZOL (DFS: HR=0.361, 95% confidence interval (CI) 0.148, 0.880; OS: HR=0.375, 95% CI 0.143, 0.985).
Conclusion:
ZOL administered with chemotherapy may improve DFS and OS in a subset of BC patients with ER− tumours. This study was not powered to compare subgroups of patients; thus, these findings should be considered hypothesis generating.
Similar content being viewed by others
Main
Breast cancer (BC) is the most commonly diagnosed malignancy and the leading cause of cancer-related mortality among women worldwide (Ferlay et al, 2010). Despite the use of neoadjuvant and adjuvant therapies in patients with localised BC, recent trials report ∼8% incidence of disease recurrence overall within the first few years after treatment, with even higher recurrence rates for patients with certain BC subtypes (Gnant et al, 2009; Eidtmann et al, 2010). The development of recurrent disease is thought to be the result of persistent micro-metastatic disease that is chemotherapy resistant (Pantel et al, 2009). The presence and persistence of disseminated tumour cells (DTCs), also known as bone marrow micro-metastases, have been associated with poor outcomes and recurrent disease in patients with early-stage BC, regardless of hormone receptor status and other established prognostic features such as nodal status (Braun et al, 2005). We and others have reported that the bone-targeted bisphosphonate, zoledronic acid (ZOL), which is currently used to treat osteoporosis and to reduce the risk of skeletal morbidity in patients with bone metastases, can also reduce the persistence of DTCs in the bone marrow of women with early BC (Lin et al, 2008; Solomayer et al, 2009; Aft et al, 2010; Rack et al, 2010).
Zoledronic acid has been reported to decrease tumour burden in the breast when administered with neoadjuvant chemotherapy (Coleman et al, 2010). In addition, we observed that subsets of patients with triple-negative BC were more likely to have a pathologic complete response (pCR) to neoadjuvant chemotherapy if they received concurrent ZOL, suggesting that bisphosphonates may provide potential anti-cancer benefits in addition to their established bone-protective activities (Neville-Webbe et al, 2010). Numerous studies have evaluated the impact of bisphosphonates on disease-free survival (DFS) and overall survival (OS) in localised BC. Although the results have been mixed, consensus is emerging that certain subsets of patients with early-stage BC may benefit from bisphosphonate therapy. Zoledronic acid administration increased DFS in premenopausal women with oestrogen receptor-positive (ER+) BC who were treated with ovarian suppression and endocrine-targeted therapies (Gnant et al, 2011a). Likewise, ZOL increased DFS in postmenopausal women with ER+ tumours who received endocrine-targeted therapies (Eidtmann et al, 2010; Coleman et al, 2011). The mechanisms of the anti-cancer effects of bisphosphonates are under intense investigation.
In this study, we report the effect of ZOL administered every 3 weeks for 1 year, beginning at the start of neoadjuvant chemotherapy, on DFS and OS outcomes in a phase II trial of 120 women with stage II/III BC, which included pre- and postmenopausal women and patients with ER+ and ER-negative (ER−) tumours (Aft et al, 2010).
Patients and methods
Patients
Eligible patients had clinical stage II/III (⩾T2 and/or ⩾N1) newly diagnosed BC with inclusion of all tumour biomarker subtypes, Eastern Cooperative Oncology Group performance status score of 0 or 1, and normal cardiac, renal and liver function. Menopausal status was defined as 1 year with no menstrual activity, previous bilateral oophorectomy, or age >56 years. Inclusion criteria for this study were as previously described (Aft et al, 2010).
Study design and treatment
This single-centre, open-label, phase II trial evaluated the efficacy and safety of adding ZOL to standard therapy in women with stage II/III BC. This study is registered with ClinicalTrials.gov, NCT00242203. Eligible women were randomly assigned to receive either 4 mg intravenous ZOL every 3 weeks for 1 year (total 17 doses) commencing with the first dose of chemotherapy, or no ZOL (chemotherapy alone; Figure 1). The randomisation process was as previously described (Aft et al, 2010).
The primary end point was the number of patients with detectable DTCs in bone marrow, measured at baseline, 3 months (after four cycles of chemotherapy), and 12 months. These results have been reported earlier (Aft et al, 2010). Respective secondary and tertiary end points were DFS, defined as the time interval between surgery (the time point of all residual disease removal) and first detectable disease recurrence or death, and OS, defined as the time from diagnosis to death from any cause or to last follow-up.
The approved dosing schedule of ZOL (4 mg via 15-min intravenous infusion every 3 weeks) for bone metastasis was used (Hillner et al, 2003). All women received four cycles of intravenous neoadjuvant epirubicin (75 mg m−2) plus docetaxel (75 mg m−2) every 3 weeks, with granulocyte-stimulating factor support and oral dexamethasone premedication (20 mg), followed by surgery and two cycles of adjuvant epirubicin plus docetaxel administered every 3 weeks. Adjuvant radiation, endocrine, and trastuzumab therapies were administered when indicated. The recommended follow-up was every 3 months for years 1 and 2 after randomisation, then every 6 months for years 3–5 after randomisation. It was recommended that all radiological exams (i.e., mammogram, computed tomography, bone or positron emission tomography) be performed annually.
All patients were encouraged to take 1000 mg calcium with 800 IU vitamin D daily. Adverse events were assessed at each follow-up. Patients were removed from the study for safety reasons, progression during chemotherapy or recurrent disease development. The Internal Review Board of Washington University approved the study, and patients provided written consent.
Study assessments
Immunostaining for ER, progesterone receptor (PgR), and human epidermal growth factor receptor-2 (HER2) was performed at Washington University. ER and PgR were considered positive if there was any detectable staining by immunohistochemistry (Ventana, Inc., Tucson, AZ, USA). HER2 was considered positive if HercepTest (Dako North America, Inc., Carpinteria, CA, USA) was 3+ or if the fluorescence in situ hybridisation (FISH) score was >2.0. The FISH analysis was done for all specimens scored as 2+ by HercepTest.
Pre-treatment tumour size was defined as the largest tumour dimension documented by mammogram, breast ultrasound, or magnetic resonance imaging. Pre-treatment lymph-node status was defined as any abnormal lymph nodes on computed tomography or ultrasound imaging, or on clinical exam, or by the presence of metastatic disease from fine-needle aspiration or sentinel lymph-node biopsy. Pathologic complete response was defined as no residual invasive tumour in the breast specimen at the time of surgery.
Statistical analysis
Kaplan–Meier estimates were generated for DFS and OS in each treatment arm, and patient subsets were defined by ER and HER2 status. Hazard ratios (HRs) and 95% confidence intervals (CIs) were calculated using Cox proportional hazards models. A propensity score, adjusting for differences in age, race, menopausal status, ER, PgR, and HER2, was found to be a significant predictor of DFS and OS; thus, all reported analyses were adjusted using the propensity score. P-values <0.05 were considered significant.
Results
Patients
Of the 120 eligible women enrolled in this study, 119 were evaluated, and of those patients ∼55% had ER+ tumours, 20% had HER2+ tumours, and 33% had ER−/HER2− tumours (Table 1; Aft et al, 2010). One patient withdrew consent before receiving treatment, one patient did not have tumour biomarkers, and two patients did not undergo surgery for their cancer. Thirty-seven patients developed recurrent disease, of whom 27 died and 10 were alive with disease at last follow-up. There were 18 deaths among the 52 ER− patients and 9 deaths among the 66 ER+ patients. The remaining 82 patients were alive without disease at last follow-up. No deaths were identified within this cohort as having a cause unrelated to BC.
Efficacy
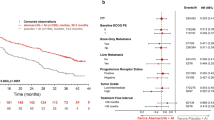
After a median follow-up of 61.9 months, DFS (P=0.92) and OS (P=0.92) were similar in the ZOL and no-ZOL arms for the overall study population (Figure 2). ER status is an independent predictor of OS (Berry et al, 2006) and, as expected in our study, times to recurrence and death were significantly different between patient subgroups defined by ER status in the no-ZOL arm (interaction P=0.010 for DFS and 0.025 for OS; Table 2). However, in the ZOL treatment arm we failed to find a differences among the ER+ and ER− patients. The hazards of disease recurrence and of death were significantly less among patients with ER− tumours who received ZOL vs those who did not (DFS: HR=0.361; 95% CI 0.148, 0.880; OS: HR=0.375; 95% CI 0.143, 0.985). There was no evidence that ZOL treatment altered DFS or OS vs no ZOL in patients with ER+ tumours (Table 3). In Kaplan–Meier analyses, there were significant differences in DFS (P=0.0007) and OS (P=0.0018) based on treatment arms (Figure 3).
As HER2+ status has significant effects on DFS and OS, especially with the recent adoption of HER2-targeted therapy, and to analyse more uniform subsets of BC patients, we analysed the effects of ER status on DFS and OS in the subset of patients with HER2− tumours (n=95). In the subset of HER2− tumours, the effect of ZOL on OS and DFS was not shown to be significantly different in ER+ and ER− patients (DFS interaction P=0.052 and OS interaction P=0.064; Table 2). However, among patients with ER−/HER2− tumours, only 58% were alive at last follow-up in the no-ZOL arm compared with 81% in the ZOL arm. The corresponding DFS rates were 47% (no ZOL) and 71% (ZOL).
Safety
As previously reported, ZOL was generally well tolerated; toxicities were similar in the two treatment groups, with no observed cases of nephrotoxicity resulting in dose modifications. One of the 60 patients (1.7%) developed osteonecrosis of the jaw after receiving 11 infusions of ZOL (Aft et al, 2010).
Discussion
With a median follow-up of 62 months, the addition of neoadjuvant ZOL to standard therapy did not significantly change median DFS or OS in women with stage II/III BC treated in this study. This is consistent with our earlier report in which we did not observe significant differences in the 1- and 2-year disease recurrence and survival rates (Aft et al, 2010). Analysis of survival rates stratified according to BC subtype revealed significant improvements in DFS and OS in women with ER− tumours randomised to receive ZOL. Our data are consistent with a recent report demonstrating a survival benefit of bisphosphonates in ER− patients with metastatic disease (Park et al, 2009). In most adjuvant trials with bisphosphonates in non-metastatic BC, the predominant tumour type is ER+. Our trial was intentionally geared to patients at high risk of metastasis; >40% of patients treated in our trial had ER− tumours and were premenopausal at diagnosis.
Three recently reported large phase III trials, which included women with all tumour subtypes, did not demonstrate an overall DFS or OS benefit from bisphosphonate treatment in women receiving adjuvant chemotherapy. These trials were the National Surgical Adjuvant Breast and Bowel Project (NSABP) B-34 trial, which compared clodronate vs placebo in women with early BC treated with adjuvant chemotherapy or endocrine therapy, the German Adjuvant Intergroup Node-positive (GAIN) study, which compared ibandronate vs placebo in women receiving adjuvant chemotherapy, and the Adjuvant Zoledronic Acid to Reduce Recurrence (AZURE) study, which compared ZOL vs placebo in women receiving adjuvant chemotherapy or endocrine therapy (Coleman et al, 2011; Mobus et al, 2011; Paterson et al, 2011). In contrast, other trials evaluating the addition of ZOL (4 mg every 6 months) to endocrine therapy demonstrated significant improvement in DFS compared with adjuvant endocrine therapy alone in premenopausal women with ovarian suppression in phase III trials (N=1803; DFS HR=0.64; P=0.01; Gnant et al, 2009) and postmenopausal (N=1065; DFS HR=0.59; P=0.03; Eidtmann et al, 2010) women with stage I to III BC. However, clinical data indicate that ER status may be a variable for clinical benefit from bisphosphonates in this setting.
In a subset analysis of the AZURE trial in patients who were unequivocally postmenopausal at the time of starting the trial, ZOL provided a benefit for DFS to those patients with ER+ tumours (Coleman et al, 2011). We await OS data from the planned subgroup analysis by tumour subtype of the NSABP B-34 and GAIN trials. Meanwhile, in the ABCSG-12 trial, those women who derived the greatest benefit from the addition of ZOL were >40 years of age at study entry (Gnant et al, 2011b). These studies suggest that women with ER+ tumours and low oestrogen levels (postmenopausal, or premenopausal women with ovarian suppression) experience a survival benefit when ZOL is administered in the adjuvant setting. In this study, we did not observe any DFS benefit with the addition of ZOL to standard therapy in the subset of patients with ER+ tumours. The lack of DFS benefit in ER+ patients may be related to the small number of events in this subgroup with a more favourable prognosis compared with ER− patients. The ER+ patients in this study were relatively young (median age, 47 years) and may have benefitted from upfront neoadjuvant chemotherapy because of their high-risk status (tumour size and other risk factors). As 60% of the patients with ER+ tumours in this trial were premenopausal at diagnosis, in contrast to the AZURE population, and were not given ovarian suppression, in contrast to the Austrian Breast and Colorectal Cancer Study Group trial 12 (ABCSG-12) population, it is difficult to extrapolate the results of our trial to others (Gnant et al, 2009).
Many bisphosphonate trials have focused on patients with ER+ disease or have not included a large population of patients with ER− disease. Few studies have examined the effects of bisphosphonates on ER− BCs. In a retrospective study, Park et al (2009) found significantly prolonged survival in ER− stage IV BC patients who received bisphosphonate treatment. In our trial, we found a significant decreased risk of recurrent disease development and death in patients with ER− disease who received ZOL (HR=0.361 and 0.375, respectively). We observed 21 recurrences among the 50 ER− patients. This population was composed of predominantly premenopausal (55%) and African American (45%) women. Thus, in contrast to ER+ tumours, the effect does not seem to be dependent on a low oestrogen environment and may be the result of a more direct anti-tumour effect of ZOL on ER− tumour cells.
In the primary report of this study, it was shown that adding ZOL to neoadjuvant chemotherapy was associated with increased rates of pCR vs no ZOL, although this difference was not significant (Aft et al, 2010). For Luminal B, HER2+, and ER−/HER2− BC subtypes, response in the breast correlates with OS, which is thought to reflect the response of systemic micro-metastatic disease (Von Minckwitz et al, 2011). Thus, patients who achieve a pCR in the breast with chemotherapy have a better prognosis than patients who have residual breast disease (Chavez-MacGregor and Gonzalez-Angulo, 2010). Pathologic complete response in the breast has been used as a surrogate for response to therapy. As previously reported, in our patient population the between-group differences in the pCR rate were most pronounced in the triple-negative subset (ER−/PgR−/HER2−; ZOL group=28%; no-ZOL group=10%), although, as with the overall population, this difference was not statistically significant (Aft et al, 2010). These data are consistent with previous clinical data from the neoadjuvant therapy subset (n=205) of the ongoing AZURE trial, wherein the addition of ZOL (4 mg every 3 to 4 weeks) to 6 cycles of neoadjuvant chemotherapy improved pCR rates approximately two-fold in a multivariate analysis of the entire neoadjuvant cohort and significantly reduced the residual invasive tumour size at surgery (relative decrease of 43%; P=0.006) vs chemotherapy alone (Coleman et al, 2010).
As previously reported, among patients without detectable DTCs at baseline, a larger proportion of ZOL-treated patients (87%) remained DTC− at 3 months compared with patients receiving chemotherapy alone (60%; P=0.03; Aft et al, 2010). Similarly, among patients who were DTC+ at baseline, a larger proportion of patients transitioned to DTC− status in the ZOL group (48%) compared with chemotherapy alone (43%; P=0.05 vs no ZOL; Aft et al, 2010). Emerging data suggest that there is a complex interaction between the tumour and bone marrow (McAllister and Weinberg, 2010). Primary tumours release cytokines that are thought to prime the bone marrow for receipt of micro-metastasis disease, interrupt the delicate balance between bone formation and destruction with the release of growth factors, and recruit bone marrow-derived cells to enhance tumour growth and invasion. Similarly, bone marrow-derived myeloid cells can promote tumour growth at primary and distant sites (Weilbaecher et al, 2011). It is possible that drugs such as ZOL affect this interaction with the observed results of tumour growth inhibition and reduction of DTCs and metastases formation (Aft, 2011).
Although multiple statistical models used in the current study show a trend of increased clinical benefit in ER− patients treated with ZOL, our findings are limited in that time to relapse (i.e., DFS) and OS were secondary and tertiary end points, respectively, and the study was not designed or powered to compare subgroups of patients. Thus, our findings should be regarded as hypothesis generating, and interpretation should be regarded with appropriate caution.
In summary, in this study, adding ZOL (4 mg every 3 weeks) to neoadjuvant chemotherapy reduced DTC persistence (Aft et al, 2010), improved pCR rates in specific patient subsets (Aft et al, 2010), and improved DFS and OS vs chemotherapy alone in the patient subset with ER− tumours. These observations in the ER− subset suggest that neoadjuvant or adjuvant ZOL may be a beneficial addition to current treatment paradigms in patients with ER− tumours, and may warrant further investigation in larger clinical trials in this high-risk patient population with few targeted therapy options.
References
Aft R (2011) Bisphosphonates in breast cancer: clinical activity and implications of preclinical data. Clin Adv Hematol Oncol 9 (3): 194–205
Aft R, Naughton M, Trinkaus K, Watson M, Ylagan L, Chavez-Macgregor M, Zhai J, Kuo S, Shannon W, Diemer K, Herrmann V, Dietz J, Ali A, Ellis M, Weiss P, Eberlein T, Ma C, Fracasso PM, Zoberi I, Taylor M, Gillanders W, Pluard T, Mortimer J, Weilbaecher K (2010) Effect of zoledronic acid on disseminated tumour cells in women with locally advanced breast cancer: an open label, randomised, phase 2 trial. Lancet Oncol 11 (5): 421–428
Berry DA, Cirrincione C, Henderson IC, Citron ML, Budman DR, Goldstein LJ, Martino S, Perez EA, Muss HB, Norton L, Hudis C, Winer EP (2006) Estrogen-receptor status and outcomes of modern chemotherapy for patients with node-positive breast cancer. JAMA 295 (14): 1658–1667
Braun S, Vogl FD, Naume B, Janni W, Osborne MP, Coombes RC, Schlimok G, Diel IJ, Gerber B, Gebauer G, Pierga JY, Marth C, Oruzio D, Wiedswang G, Solomayer EF, Kundt G, Strobl B, Fehm T, Wong GY, Bliss J, Vincent-Salomon A, Pantel K (2005) A pooled analysis of bone marrow micrometastasis in breast cancer. N Engl J Med 353 (8): 793–802
Chavez-MacGregor M, Gonzalez-Angulo AM (2010) Breast cancer, neoadjuvant chemotherapy and residual disease. Clin Transl Oncol 12 (7): 461–467
Coleman RE, Marshall H, Cameron D, Dodwell D, Burkinshaw R, Keane M, Gil M, Houston SJ, Grieve RJ, Barrett-Lee PJ, Ritchie D, Pugh J, Gaunt C, Rea U, Peterson J, Davies C, Hiley V, Gregory W, Bell R (2011) Breast-cancer adjuvant therapy with zoledronic acid. N Engl J Med 365 (15): 1396–1405
Coleman RE, Winter MC, Cameron D, Bell R, Dodwell D, Keane MM, Gil M, Ritchie D, Passos-Coelho JL, Wheatley D, Burkinshaw R, Marshall SJ, Thorpe H (2010) The effects of adding zoledronic acid to neoadjuvant chemotherapy on tumour response: exploratory evidence for direct anti-tumour activity in breast cancer. Br J Cancer 102 (7): 1099–1105
Eidtmann H, de Boer R, Bundred N, Llombart-Cussac A, Davidson N, Neven P, von Minckwitz G, Miller J, Schenk N, Coleman R (2010) Efficacy of zoledronic acid in postmenopausal women with early breast cancer receiving adjuvant letrozole: 36-month results of the ZO-FAST Study. Ann Oncol 21 (11): 2188–2194
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM (2010) Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 127 (12): 2893–2917
Gnant M, Mlineritsch B, Schippinger W, Luschin-Ebengreuth G, Postlberger S, Menzel C, Jakesz R, Seifert M, Hubalek M, Bjelic-Radisic V, Samonigg H, Tausch C, Eidtmann H, Steger G, Kwasny W, Dubsky P, Fridrik M, Fitzal F, Stierer M, Rucklinger E, Greil R, Marth C (2009) Endocrine therapy plus zoledronic acid in premenopausal breast cancer. N Engl J Med 360 (7): 679–691
Gnant M, Mlineritsch B, Stoeger H, Luschin-Ebengreuth G, Heck D, Menzel C, Jakesz R, Seifert M, Hubalek M, Pristauz G, Bauernhofer T, Eidtmann H, Eiermann W, Steger G, Kwasny W, Dubsky P, Hochreiner G, Forsthuber EP, Fesl C, Greil R (2011a) Adjuvant endocrine therapy plus zoledronic acid in premenopausal women with early-stage breast cancer: 62-month follow-up from the ABCSG-12 randomised trial. Lancet Oncol 12 (7): 631–641
Gnant M, Mlineritsch B, Stoeger H, Luschin-Ebengreuth G, Poestlberger S, Dubsky PC, Jakesz R, Singer CF, Eidtmann H, Greil R (2011b) Overall survival with adjuvant zoledronic acid in patients with premenopausal breast cancer with complete endocrine blockade: long-term results from ABCSG-12 (abstract). J Clin Oncol 29 (Suppl): Abstract 520
Hillner BE, Ingle JN, Chlebowski RT, Gralow J, Yee GC, Janjan NA, Cauley JA, Blumenstein BA, Albain KS, Lipton A, Brown S (2003) American Society of Clinical Oncology 2003 update on the role of bisphosphonates and bone health issues in women with breast cancer. J Clin Oncol 21 (21): 4042–4057
Lin AY, Park JW, Scott J, Melisko M, Goga A, Moasser MM, Moore DH, Rugo HS (2008) Zoledronic acid as adjuvant therapy for women with early stage breast cancer and disseminated tumor cells in bone marrow (abstract). J Clin Oncol 26 (S15): 559
McAllister SS, Weinberg RA (2010) Tumor-host interactions: a far-reaching relationship. J Clin Oncol 28 (26): 4022–4028
Mobus V, Diel IJ, Elling D, Harbeck N, Jackisch C, Thomssen C, Untch M, Conrad B, Schneeweiss A, Kreienberg R, Huober J, Muller V, Luck HJ, Bauerfeind I, Loibl S, Nekljudova V, von Minckwitz G (2011) GAIN study: a phase III trial to compare ETC vs EC-TX and ibandronate vs observation in patients with node-positive primary breast cancer – 1st interim efficacy analysis (abstract). 34th Annual San Antonio Breast Cancer Symposium 6–10 December, 2011; San Antonio, TX. Abstract S2–4
Neville-Webbe HL, Gnant M, Coleman RE (2010) Potential anticancer properties of bisphosphonates. Semin Oncol 37 (Suppl 1): S53–S65
Pantel K, Alix-Panabieres C, Riethdorf S (2009) Cancer micrometastases. Nat Rev Clin Oncol 6 (6): 339–351
Park IH, Ro J, Nam BH, Kwon Y, Lee KS (2009) Potential antitumor effects of nitrogen-containing bisphosphonate in hormone receptor negative breast cancer patients with bone metastases. BMC Cancer 9: 154
Paterson AHG, Anderson SJ, Lembersky BC, Fehrenbacher L, Falkson CI, King KM, Weir LM, Brufsky AM, Dakhil S, Lad T, Baez-Diaz L, Gralow JR, Robidoux A, Perez EA, Zheng P, Geyer CE, Swain SM, Costantino JP, Mamounas EP, Wolmark N (2011) NSABP protocol B-34: a clinical trial comparing adjuvant clodronate vs placebo in early stage breast cancer patients receiving systemic chemotherapy and/or tamoxifen or no therapy—final analysis. 34th Annual San Antonio Breast Cancer Symposium 6–10 December, 2011; San Antonio, TX. Abstract S2–3
Rack B, Juckstock J, Genss EM, Schoberth A, Schindlbeck C, Strobl B, Heinrigs M, Rammel G, Zwingers T, Sommer H, Friese K, Janni W (2010) Effect of zoledronate on persisting isolated tumour cells in patients with early breast cancer. Anticancer Res 30 (5): 1807–1813
Solomayer E, Gebauer G, Hirnle P, Janni W, Lück H-J, Becker S, Huober J, Kraemer B, Wackwitz B, Fehm T (2009) Influence of zoledronic acid on disseminated tumor cells (DTC) in primary breast cancer patients (abstract). Cancer Res 69 (2 Suppl 1): 170s–171s, . Abstract 2048
Von Minckwitz G, Kaufmann M, Kuemmel S, Fasching PA, Eiermann W, Blohmer JU, Costa SD, Hilfrich J, Jackisch C, Gerber B, Du Bois A, Huober JB, Hanusch CA, Konecny GE, Fett W, Stickeler E, Harbeck N, Mehta K, Loibl S, Untch M (2011) Correlation of various pathologic complete response (pCR) definitions with long-term outcome and the prognostic value of pCR in various breast cancer subtypes: results from the German neoadjuvant meta-analysis. J Clin Oncol 29 (S15): 1028
Weilbaecher KN, Guise TA, McCauley LK (2011) Cancer to bone: a fatal attraction. Nat Rev Cancer 11 (6): 411–425
Acknowledgements
We would like to thank our patients and their families for being active and enthusiastic participants in this study. We thank Ms Susan Fox and Ms Farley Johnson who provided outstanding assistance with the data and clinical trial management. We would also like to thank the doctors and nurses of Surgical Oncology, Medical Oncology, and Radiation Oncology at the Washington University School of Medicine and Siteman Cancer Center for the exceptional care provided to study patients. Research support was provided by KNW (R01-CA097250, PPG-CA100730), St Louis Men’s Group against Cancer. Financial support for medical editorial assistance was provided by Novartis Pharmaceuticals Corporation. We thank Jerome F Sah, PhD, ProEd Communications, Inc., for his medical editorial assistance with this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
R Aft and M Naughton have received honoraria from Novartis. The remaining authors have no conflict of interest.
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Aft, R., Naughton, M., Trinkaus, K. et al. Effect of (Neo)adjuvant zoledronic acid on disease-free and overall survival in clinical stage II/III breast cancer. Br J Cancer 107, 7–11 (2012). https://doi.org/10.1038/bjc.2012.210
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2012.210
Keywords
This article is cited by
-
Long-term outcome of (neo)adjuvant zoledronic acid therapy in locally advanced breast cancer
Breast Cancer Research and Treatment (2021)
-
Long-term outcomes of prolonged bisphosphonates more than 2 years in bone metastatic breast cancer: risk vs benefit
Irish Journal of Medical Science (1971 -) (2020)
-
The efficacy and safety of zoledronic acid and strontium-89 in treating non–small cell lung cancer: a systematic review and meta-analysis of randomized controlled trials
Supportive Care in Cancer (2020)
-
The differential anti-tumour effects of zoledronic acid in breast cancer – evidence for a role of the activin signaling pathway
BMC Cancer (2015)
-
Adjuvant zoledronic acid therapy for patients with early stage breast cancer: an updated systematic review and meta-analysis
Journal of Hematology & Oncology (2013)