Abstract
Background
Higher survival rates for breast cancer patients have led to concerns in dealing with short- and long-term side effects. The most common complications are impairment of shoulder functions, pain, lymphedema, and dysesthesia of the injured arm; psychological consequences concern: emotional distress, anxiety, and depression, thereby, deeply impacting/affecting daily living activity, and health-related quality of life.
Objective
To perform a systematic review for assessing the efficacy or effectiveness of interventions aiming at improving health-related quality of life, return to daily activity, and correct lifestyles among breast cancer patients.
Methods
A literature search was conducted in December 2016 using the databases PubMed and Scopus. Search terms included: (counseling) AND (breast cancer) AND (quality of life). Articles on counseling interventions to improve quality of life, physical and psychological outcomes were included.
Results
Thirty-five articles met the inclusion criteria. The interventions were grouped in five main areas: concerning lifestyle counseling interventions, related to combined interventions (physical activity and nutritional counseling), physical therapy, peer counseling, multidisciplinary approach, included psychological, psycho-educational interventions, and cognitive-behavior therapy (CBT). Exercise counseling as well as physical therapy are effective to improve shoulder mobility, healing wounds, and limb strength. Psychological therapies such as psychoeducation and CBT may help to realize a social and psychological rehabilitation.
Conclusion
A multidisciplinary approach can help in sustaining and restoring impaired physical, psychosocial, and occupational outcomes of breast cancer patients.

Similar content being viewed by others
References
Torre, L. A., Bray, F., Siegel, R. L., Ferlay, J., Lortet-Tieulent, J., & Jemal, A. (2015). Global cancer statistics, 2012. CA: A Cancer Journal for Clinicians, 65(2), 87–108.
AIOM-AIRTUM. I numeri del cancro in Italia 2015. Intermedia Editor, http://www.registritumori.it/PDF/AIOM2015/I_numeri_del_cancro_2015.pdf.
Chung, C., Lee, S., Hwang, S., & Park, E. (2013). Systematic review of exercise effects on health outcomes in women with breast cancer. Asian Nursing Research, 7(3), 149–159.
Hayes, S. C., Johansson, K., Stout, N. L., Prosnitz, R., Armer, J. M., Gabram, S., et al. (2012). Upper-body morbidity after breast cancer. Cancer, 118(S8), 2237–2249.
van’t Spijker, A., Trijsburg, R. W., & Duivenvoorden, H. (1997). Psychological sequelae of cancer diagnosis: a meta-analytical review of 58 studies after 1980. Psychosomatic Medicine, 59(3), 280–293.
Bradley, C. J., Bednarek, H. L., & Neumark, D. (2002). Breast cancer survival, work, and earnings. Journal of Health Economics, 21(5), 757–779.
Fu, M. R., Chen, C. M., Haber, J., Guth, A. A., & Axelrod, D. (2010). The effect of providing information about lymphedema on the cognitive and symptom outcomes of breast cancer survivors. Annals of Surgical Oncology, 17(7), 1847–1853.
Bo Bowling, A. (1995). What things are important in people’s lives? A survey of the public’s judgements to inform scales of health related quality of life. Social Science and Medicine, 41(10), 1447–1462.
World Cancer Research Fund/American Institute for Cancer Research. Continuous update project report. Food, nutrition, physical activity, and the prevention of breast cancer (2010).
World Cancer Research Fund/American Institute for Cancer Research. (2007). Food, nutrition, physical activity, and the prevention of cancer: A global perspective. Washington, DC: AICR.
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., & PRISMA Group. (2010). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. International Journal of Surgery, 8(5), 336–341.
Wells, G. A., Shea, B., O'Connell, D., Peterson, J., Welch V, Losos, M., et al. (2011). The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses.
Jadad, A. R., Moore, R. A., Carroll, D., Jenkinson, C., Reynolds, D. J. M., Gavaghan, D. J., et al. (1996). Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Controlled Clinical Trials, 17(1), 1–12.
Shea, B. J., Grimshaw, J. M., Wells, G. A., Boers, M., Andersson, N., Hamel, C., et al. (2007). Development of AMSTAR: A measurement tool to assess the methodological quality of systematic reviews. BMC Medical Research Methodology, 7(1), 10.
La Torre, G., Backhaus, I., & Mannocci, A. (2015). Rating for narrative reviews: Concept and development of the International Narrative Systematic Assessment tool. Senses Sci, 2, 31–35.
Akechi, T., Momino, K., Miyashita, M., Sakamoto, N., Yamashita, H., & Toyama, T. (2015). Anxiety in disease-free breast cancer patients might be alleviated by provision of psychological support, not of information. Japanese Journal of Clinical Oncology, 45(10), 929–933. doi:10.1093/jjco/hyv112.
Fallowfield, L. J. (1993). Quality of life measurement in breast cancer. Journal of the Royal Society of Medicine, 86(1), 10–12.
Axelrod, D., Smith, J., Kornreich, D., Grinstead, E., Singh, B., Cangiarella, J., et al. (2008). Breast cancer in young women. Journal of the American College of Surgeons, 206(6), 1193–1203.
Boinon, D., Sultan, S., Charles, C., Stulz, A., Guillemeau, C., Delaloge, S., et al. (2014). Changes in psychological adjustment over the course of treatment for breast cancer: The predictive role of social sharing and social support. Psycho-Oncology, 23(3), 291–298.
Loh, S. Y. (2012). Improving cancer survivorships: Targeting physical activity and inactivity at teachable moments. Journal of University of Malaya Medical Centre (JUMMEC), 15(1), 1–6.
Bowen, D. J., & Powers, D. (2010). Effects of a mail and telephone intervention on breast health behaviors. Health Education & Behavior, 37(4), 479–489.
Kawaguchi, T., Iwase, S., Koinuma, M., Onodera, Y., Takeuchi, H., Umeda, M., et al. (2011). Determinants affecting quality of life: Implications for pharmacist counseling for patients with breast cancer in Japan. Biological & Pharmaceutical Bulletin, 35(1), 59–64.
Baruth, M., Wilcox, S., Ananian, C. D., & Heiney, S. (2015). Effects of home-based walking on quality of life and fatigue outcomes in early stage breast cancer survivors: A 12-week pilot study. Journal of Physical Activity and Health, 12(s1), S110–S118.
Jones, L. W., & Courneya, K. S. (2002). Exercise counseling and programming preferences of cancer survivors. Cancer Practice, 10(4), 208–215.
McCarroll, M. L., Armbruster, S., Pohle-Krauza, R. J., Lyzen, A. M., Min, S., Nash, D., et al. (2015). Feasibility of a lifestyle intervention for overweight/obese endometrial and breast cancer survivors using an interactive mobile application. Gynecologic Oncology, 137(3), 508–515.
Barden, S. M., Gutierrez, D., Gonzalez, J., & Ali, S. (2016). Healing faith: A qualitative exploration of latina breast cancer survivors. Counseling and Values, 61(2), 142–158.
Larsson, J., Sandelin, K., & Forsberg, C. (2010). Health-related quality of life and healthcare experiences in breast cancer patients in a study of Swedish women. Cancer Nursing, 33(2), 164–170.
Montazeri, A. (2008). Health-related quality of life in breast cancer patients: A bibliographic review of the literature from 1974 to 2007. Journal of Experimental & Clinical Cancer Research, 27(1), 32.
Uster, A., Ruefenacht, U., Ruehlin, M., Pless, M., Siano, M., Haefner, M., et al. (2013). Influence of a nutritional intervention on dietary intake and quality of life in cancer patients: A randomized controlled trial. Nutrition, 29(11), 1342–1349.
Ganz, P. A., Rowland, J. H., Desmond, K., Meyerowitz, B. E., & Wyatt, G. E. (1998). Life after breast cancer: Understanding women’s health-related quality of life and sexual functioning. Journal of Clinical Oncology, 16(2), 501–514.
Knols, R. H., de Bruin, E. D., Shirato, K., Uebelhart, D., & Aaronson, N. K. (2010). Physical activity interventions to improve daily walking activity in cancer survivors. BMC Cancer, 10(1), 406.
Dizon, D. S. (2009). Quality of life after breast cancer: Survivorship and sexuality. The Breast Journal, 15(5), 500–504.
Demark-Wahnefried, W., Rogers, L. Q., Alfano, C. M., Thomson, C. A., Courneya, K. S., Meyerhardt, J. A., et al. (2015). Practical clinical interventions for diet, physical activity, and weight control in cancer survivors. CA: A Cancer Journal for Clinicians, 65(3), 167–189.
Pockaj, B. A., Degnim, A. C., Boughey, J. C., Gray, R. J., McLaughlin, S. A., & Dueck, A. C. (2009). Quality of life after breast cancer surgery: What have we learned and where should we go next? Journal of Surgical Oncology, 99(7), 447–455.
Fallowfield, L. J. (1995). Assessment of quality of life in breast cancer. Acta Oncologica, 34(5), 689–694.
Jassim, G. A., & Whitford, D. L. (2013). Quality of life of Bahraini women with breast cancer: A cross sectional study. BMC Cancer, 13(1), 212.
Badger, T. A., Segrin, C., Hepworth, J. T., Pasvogel, A., Weihs, K., & Lopez, A. M. (2013). Telephone-delivered health education and interpersonal counseling improve quality of life for Latinas with breast cancer and their supportive partners. Psycho-Oncology, 22(5), 1035–1042.
Rock, C. L., Doyle, C., Demark-Wahnefried, W., Meyerhardt, J., Courneya, K. S., Schwartz, A. L., et al. (2012). Nutrition and physical activity guidelines for cancer survivors. CA: A Cancer Journal for Clinicians, 62(4), 242–274.
Lahart, I. M., Metsios, G. S., Nevill, A. M., Kitas, G. D., & Carmichael, A. R. (2016). Randomised controlled trial of a home-based physical activity intervention in breast cancer survivors. BMC Cancer, 16(1), 234.
Darga, L. L., Magnan, M., Mood, D., Hryniuk, W. M., DiLaura, N. M., & Djuric, Z. (2007). Quality of life as a predictor of weight loss in obese, early-stage breast cancer survivors. Oncology Nursing Forum, 34(1), 86–92.
Cho, S. W., Kim, J. H., Lee, S. M., Lee, S. M., Choi, E. J., Jeong, J., et al. (2014). Effect of 8-week nutrition counseling to increase phytochemical rich fruit and vegetable consumption in korean breast cancer patients: A randomized controlled trial. Clinical Nutrition Research, 3(1), 39–47.
Pi-Sunyer, F. X., Becker, D. M., Bouchard, C., Carleton, R. A., Colditz, G. A., Dietz, W. H., et al. (1998). Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. American Journal of Clinical Nutrition, 68(4), 899–917.
Befort, C. A., Klemp, J. R., Austin, H. L., Perri, M. G., Schmitz, K. H., Sullivan, D. K., et al. (2012). Outcomes of a weight loss intervention among rural breast cancer survivors. Breast Cancer Research and Treatment, 132(2), 631–639.
Demark-Wahnefried, W., Clipp, E. C., Morey, M. C., Pieper, C. F., Sloane, R., Snyder, D. C., et al. (2004). Physical function and associations with diet and exercise: Results of a cross-sectional survey among elders with breast or prostate cancer. International Journal of Behavioral Nutrition and Physical Activity, 1(1), 16.
Demark-Wahnefried, W., Morey, M. C., Sloane, R., Snyder, D. C., & Cohen, H. J. (2009). Promoting healthy lifestyles in older cancer survivors to improve health and preserve function. Journal of the American Geriatrics Society, 57(s2), s262–s264.
Carayol, M., Romieu, G., Bleuse, J. P., Senesse, P., Gourgou-Bourgade, S., Sari, C., et al. (2013). Adapted physical activity and diet (APAD) during adjuvant breast cancer therapy: Design and implementation of a prospective randomized controlled trial. Contemporary Clinical Trials, 36(2), 531–543.
Gnagnarella, P., Dragà, D., Baggi, F., Simoncini, M. C., Sabbatini, A., Mazzocco, K., et al. (2016). Promoting weight loss through diet and exercise in overweight or obese breast cancer survivors (InForma): Study protocol for a randomized controlled trial. Trials, 17(1), 363.
Spector, D., Battaglini, C., Alsobrooks, A., Owen, J., & Groff, D. (2012). Do breast cancer survivors increase their physical activity and enhance their health-related quality of life after attending community-based wellness workshops? Journal of Cancer Education, 27(2), 353–361.
Naumann, F., Martin, E., Philpott, M., Smith, C., Groff, D., & Battaglini, C. (2012). Can counseling add value to an exercise intervention for improving quality of life in breast cancer survivors? A feasibility study. The Journal of Supportive Oncology, 10(5), 188–194.
http://www.acsm.org/public-information/articles/2016/10/07/exercise-during-cancer-treatment.
Casla, S., Hojman, P., Cubedo, R., Calvo, I., Sampedro, J., & Barakat, R. (2014). Integrative exercise and lifestyle intervention increases leisure-time activity in breast cancer patients. Integrative Cancer Therapies, 13(6), 493–501.
Demark-Wahnefried, W., Colditz, G. A., Rock, C. L., Sedjo, R. L., Liu, J., Wolin, K. Y., et al. (2015). Quality of life outcomes from the exercise and nutrition enhance recovery and good health for you (ENERGY)-randomized weight loss trial among breast cancer survivors. Breast Cancer Research and Treatment, 154(2), 329–337.
Rogers, L. Q., Courneya, K. S., Anton, P. M., Hopkins-Price, P., Verhulst, S., Vicari, S. K., et al. (2015). Effects of the BEAT Cancer physical activity behavior change intervention on physical activity, aerobic fitness, and quality of life in breast cancer survivors: A multicenter randomized controlled trial. Breast Cancer Research and Treatment, 149(1), 109–119.
Chan, D. N., Lui, L. Y., & So, W. K. (2010). Effectiveness of exercise programmes on shoulder mobility and lymphoedema after axillary lymph node dissection for breast cancer: Systematic review. Journal of Advanced Nursing, 66(9), 1902–1914.
McNeely, M. L., Campbell, K., Ospina, M., Rowe, B. H., Dabbs, K., Klassen, T. P., et al. (2010). Exercise interventions for upper-limb dysfunction due to breast cancer treatment. The Cochrane Library, 6, CD005211.
Paramanandam, V. S., & Roberts, D. (2014). Weight training is not harmful for women with breast cancer-related lymphoedema: A systematic review. Journal of Physiotherapy, 60(3), 136–143.
cancer.org [homepage on the Internet]. American Cancer Society Cancer Facts and Figures 2012. Atlanta: American Cancer Society. Retrieved January 31, 2015, from http://www.cancer.org/research/cancerfactsfigures/cancerfactsfigures/cancer-facts-figures-2012
Loh, S. Y., & Musa, A. N. (2015). Methods to improve rehabilitation of patients following breast cancer surgery: A review of systematic reviews. Breast Cancer: Targets and Therapy, 7, 81.
Martin-Diener, E., & Martin, B. W. (2009). Two base documents for Switzerland:” Health-Enhancing Physical Activity” and” Muscle-Powered Mobility”. Schweizerische Zeitschrift fur Sportmedizin und Sporttraumatologie, 57(2), 44.
Giese-Davis, J., Bliss-Isberg, C., Wittenberg, L., White, J., Star, P., Zhong, L., et al. (2016). Peer-counseling for women newly diagnosed with breast cancer: A randomized community/research collaboration trial. Cancer, 122(15), 2408–2417.
Giese-Davis, J., Bliss-Isberg, C., Carson, K., Star, P., Donaghy, J., Cordova, M. J., et al. (2006). The effect of peer counseling on quality of life following diagnosis of breast cancer: An observational study. Psycho-Oncology, 15(11), 1014–1022.
Sharif, F., Abshorshori, N., Tahmasebi, S., Hazrati, M., Zare, N., & Masoumi, S. (2010). The effect of peer-led education on the life quality of mastectomy patients referred to breast cancer-clinics in Shiraz, Iran 2009. Health and Quality of Life Outcomes, 8(1), 74.
Marcus, A. C., Garrett, K. M., Cella, D., Wenzel, L. B., Brady, M. J., Crane, L. A., et al. (1998). Telephone counseling of breast cancer patients after treatment: A description of a randomized clinical trial. Psycho-Oncology, 7(6), 470–482.
Marcus, A. C., Garrett, K. M., Cella, D., Wenzel, L., Brady, M. J., Fairclough, D., et al. (2010). Can telephone counseling post-treatment improve psychosocial outcomes among early stage breast cancer survivors? Psycho-Oncology, 19(9), 923–932.
Prochaska, J. O., & Velicer, W. F. (1997). The transtheoretical model of health behavior change. American Journal of Health Promotion, 12(1), 38–48.
Kim, S. H., Shin, M. S., Lee, H. S., Lee, E. S., Ro, J. S., Kang, H. S., et al. (2011). Randomized pilot test of a simultaneous stage-matched exercise and diet intervention for breast cancer survivors. Oncology Nursing Forum, 38(2), E97–E106.
National Cancer Institute. (2009). Eating Hints— National Cancer Institute. Washington, DC: National Cancer Institute.
Badger, T., Segrin, C., Pasvogel, A., & Lopez, A. M. (2013). The effect of psychosocial interventions delivered by telephone and videophone on quality of life in early-stage breast cancer survivors and their supportive partners. Journal of Telemedicine and Telecare, 19(5), 260–265.
Badger, T., Segrin, C., Meek, P., Lopez, A. M., & Bonham, E. (2004). A case study of telephone interpersonal counseling for women with breast cancer and their partners. In Oncology Nursing Forum (Vol. 31, No. 5, pp. 997–1003). 125 enterprise dr, pittsburgh, PA 15275 USA: Oncology Nursing Society.
Badger, T., Segrin, C., Meek, P., Lopez, A. M., Bonham, E., & Sieger, A. (2005,). Telephone interpersonal counseling with women with breast cancer: symptom management and quality of life. In Oncology Nursing Forum-Oncology Nursing Society (Vol. 32, No. 2, pp. 273–280). [Pittsburgh, PA, etc.] Oncology Nursing Society
Badger, T., Segrin, C., Meek, P., Lopez, A. M., & Bonham, E. (2006). Profiles of women with breast cancer: Who responds to a telephone interpersonal counseling intervention? Journal of Psyhosocical Oncology, 23(2–3), 79–100.
David, N., Schlenker, P., Prudlo, U., & Larbig, W. (2011). Online counseling via e-mail for breast cancer patients on the German internet: Preliminary results of a psychoeducational intervention. GMS Psycho-Social-Medicine, 8, 5.
Gellert, G. A., Maxwell, R. M., & Siegel, B. S. (1993). Survival of breast cancer patients receiving adjunctive psychosocial support therapy: A 10-year follow-up study. Journal of Clinical Oncology, 11(1), 66–69.
Marchioro, G., Azzarello, G., Checchin, F., Perale, M., Segati, R., Sampognaro, E., et al. (1996). The impact of a psychological intervention on quality of life in non-metastatic breast cancer. European Journal of Cancer, 32(9), 1612–1615.
Lee, H., Lim, Y., Yoo, M. S., & Kim, Y. (2011). Effects of a nurse-led cognitive-behavior therapy on fatigue and quality of life of patients with breast cancer undergoing radiotherapy: An exploratory study. Cancer Nursing, 34(6), E22–E30.
Gonçalves, V. (2011). Counselling and cognitive behaviour interventions delivered to reduce psychological morbidity and improve quality of life in gynaecological cancer patients: Recent achievements. Current Women’s Health Reviews, 7(4), 391–404.
Arving, C., Thormodsen, I., Brekke, G., Mella, O., Berntsen, S., & Nordin, K. (2013). Early rehabilitation of cancer patients—a randomized controlled intervention study. BMC Cancer, 13(1), 9.
Maeda, T., Kurihara, H., Morishima, I., & Munakata, T. (2008). The effect of psychological intervention on personality change, coping, and psychological distress of Japanese primary breast cancer patients. Cancer Nursing, 31(4), E27–E35.
Hoving, J. L., Broekhuizen, M. L. A., & Frings-Dresen, M. H. W. (2009). Return to work of breast cancer survivors: A systematic review of intervention studies. BMC Cancer, 9(1), 117.
de Boer, A. G., Taskila, T. K., Tamminga, S. J., Frings-Dresen, M. H., Feuerstein, M., & Verbeek, J. H. (2011). Interventions to enhance return-to-work for cancer patients. The Cochrane Library, 19(9), 1429–1439.
Rogers, L. Q., Markwell, S., Hopkins-Price, P., Vicari, S., Courneya, K. S., Hoelzer, K., et al. (2011). Reduced barriers mediated physical activity maintenance among breast cancer survivors. Journal of Sport and Exercise Psychology, 33(2), 235–254.
Freeman, A., & Reinecke, M. A. (1995). Cognitive therapy. In A. S. Gurman, S. B. Messer, (Eds), Essential Psychotherapies. Theory and Practice. New York, NY: The Guilford Press; 182Y225.
Prochaska, J. O., & DiClemente, C. C. (1983). Stages and processes of self-change of smoking: toward an integrative model of change. Journal of Consulting and Clinical Psychology, 51(3), 390–395
Andersen, B. L., (2002) Biobehavioral outcomes following psychological interventions for cancer patients. Journal of Consulting and Clinical Psychology, 70(3), 590–610
Funding
This work was not supported by other organizations.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Appendices
Annex 1: PICOS inclusion and exclusion criteria
Inclusion criteria | Exclusion criteria | |
|---|---|---|
Population | Women with diagnosis of breast cancer | Children and adolescents, patients with other solid cancer |
Interventions | 1. Lifestyle intervention counseling: nutritional—change in dietary habits, dietary regime, physical activity habits; physical exercise: home-based and instructed exercise, supervised training program by qualified exercise physiologist; group session of exercise, and diet 2. Comple—combined interventions, e.g., counseling and exercise 3. Physical therapy: manual lymph drainage (MLD), standard physiotherapy 4. Peer counseling, familiar counseling 5. Psychological intervention: cognitive-behavior therapy (CBT), psychoeducation, psychological counseling conducted face-to face or through telephone: telephone interpersonal counseling (TIP-C), telephone health education (THE), telephone psychosocial intervention (TTM Prochaska e Di Clemente, other complex protocols) | Alternative medicine—e.g., Chinese medicine herbal |
Comparator (e.g., control) | Usual care | No intervention applied |
Outcomes | Primary: HrQoL, Secondary: Physical (e.g., lymphedema, shoulder mobility) Psychosocial (e.g., anxiety, depression, psychological well-being, affect/mood,) Occupational (e.g., return to work, lifestyle) | Article not including HrQoL as outcome |
Study design | RCT, observational studies, narrative review, systematic review, review of systematic review, no restriction of language | None |
Annex 2 Prisma Statement Checklist
Section/topic | # | Checklist item | Reported on page # |
|---|---|---|---|
Title | |||
Title | 1 | Identify the report as a systematic review, meta-analysis, or both | 1 |
Abstract | |||
Structured summary | 2 | Provide a structured summary including, as applicable: background; objectives; data sources; study eligibility criteria, participants, and interventions; study appraisal and synthesis methods; results; limitations; conclusions and implications of key findings; systematic review registration number | 2 |
Introduction | |||
Rationale | 3 | Describe the rationale for the review in the context of what is already known | 3 |
Objectives | 4 | Provide an explicit statement of questions being addressed with reference to participants, interventions, comparisons, outcomes, and study design (PICOS) | 3 |
Methods | |||
Protocol and registration | 5 | Indicate if a review protocol exists, if and where it can be accessed (e.g., Web address), and, if available, provide registration information including registration number | 4 |
Eligibility criteria | 6 | Specify study characteristics (e.g., PICOS, length of follow-up) and report characteristics (e.g., years considered, language, publication status) used as criteria for eligibility, giving rationale | 4 |
Information sources | 7 | Describe all information sources (e.g., databases with dates of coverage, contact with study authors to identify additional studies) in the search and date last searched | 4 |
Search | 8 | Present full electronic search strategy for at least one database, including any limits used, such that it could be repeated | 4 |
Study selection | 9 | State the process for selecting studies (i.e., screening, eligibility, included in systematic review, and, if applicable, included in the meta-analysis) | 4 |
Data collection process | 10 | Describe method of data extraction from reports (e.g., piloted forms, independently, in duplicate) and any processes for obtaining and confirming data from investigators | 5 |
Data items | 11 | List and define all variables for which data were sought (e.g., PICOS, funding sources) and any assumptions and simplifications made | 4 |
Risk of bias in individual studies | 12 | Describe methods used for assessing risk of bias of individual studies (including specification of whether this was done at the study or outcome level), and how this information is to be used in any data synthesis | n.a. |
Summary measures | 13 | State the principal summary measures (e.g., risk ratio, difference in means) | n.a. |
Synthesis of results | 14 | Describe the methods of handling data and combining results of studies, if done, including measures of consistency (e.g., I2) for each meta-analysis | n.a. |
Section/topic | # | Checklist item | Reported on page # |
Risk of bias across studies | 15 | Specify any assessment of risk of bias that may affect the cumulative evidence (e.g., publication bias, selective reporting within studies) | n.a. |
Additional analyses | 16 | Describe methods of additional analyses (e.g., sensitivity or subgroup analyses, meta-regression), if done, indicating which were prespecified | n.a. |
Results | |||
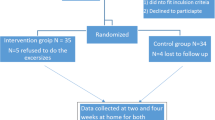
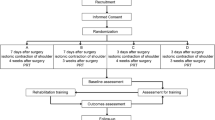
Study selection | 17 | Give numbers of studies screened, assessed for eligibility, and included in the review, with reasons for exclusions at each stage, ideally with a flow diagram | 6;8 |
Study characteristics | 18 | For each study, present characteristics for which data were extracted (e.g., study size, PICOS, follow-up period) and provide the citations | 8–24 |
Risk of bias within studies | 19 | Present data on risk of bias of each study and, if available, any outcome level assessment (see item 12) | n.a. |
Results of individual studies | 20 | For all outcomes considered (benefits or harms), present, for each study: (a) simple summary data for each intervention group, (b) effect estimates and confidence intervals, ideally with a forest plot | 8–24 |
Synthesis of results | 21 | Present results of each meta-analysis done, including confidence intervals and measures of consistency. | 8–24 |
Risk of bias across studies | 22 | Present results of any assessment of risk of bias across studies (see Item 15) | n.a. |
Additional analysis | 23 | Give results of additional analyses, if done (e.g., sensitivity or subgroup analyses, meta-regression [see Item 16]) | n.a. |
Discussion | |||
Summary of evidence | 24 | Summarize the main findings including the strength of evidence for each main outcome; consider their relevance to key groups (e.g., healthcare providers, users, and policy makers) | 25–28 |
Limitations | 25 | Discuss limitations at study and outcome level (e.g., risk of bias), and at review-level (e.g., incomplete retrieval of identified research, reporting bias) | 27 |
Conclusions | 26 | Provide a general interpretation of the results in the context of other evidence, and implications for future research | 28 |
Funding | |||
Funding | 27 | Describe sources of funding for the systematic review and other support (e.g., supply of data); role of funders for the systematic review | 28 |
Annex 3: Interventions included and main outcomes
Author | Interventions | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
Nutritional | Physical activity | Combined | Physiotherapy | Peer counseling | Multidisciplinary | Psychological | Psychosocial | TIP-C | THE | CBT | |
Gellert [73] | x | ||||||||||
Marchioro [74] | x | ||||||||||
Marcus [63] | x | ||||||||||
Darga [40] | x | ||||||||||
Andersen [84] | x | x | |||||||||
Badger [69] | x | ||||||||||
Badger [70] | x | ||||||||||
Badger [70] | x | ||||||||||
Giese-Davis [61] | x | ||||||||||
Maeda [78] | x | ||||||||||
Demark-Wahnefried [45] | x | ||||||||||
Sharif [62] | x | ||||||||||
Hoving [79] | x | ||||||||||
Marcus [64] | x | ||||||||||
Lee [75] | x | ||||||||||
David [72] | x | ||||||||||
Gonçalves [76] | x | ||||||||||
Naumann [49] | x | ||||||||||
De Boer [80] | |||||||||||
Kim [66] | x | ||||||||||
Spector [48] | x | ||||||||||
Befort [43] | x | ||||||||||
McCarroll [25] | x | ||||||||||
Badger [37] | x | x | |||||||||
Arving [77] | x | ||||||||||
Carayol [46] | x | ||||||||||
Casla [51] | x | ||||||||||
Cho [41] | x | ||||||||||
Demark-Wahnefried [52] | x | ||||||||||
Rogers [53] | x | ||||||||||
Loh [58] | x | x | x | x | x | x | x | x | |||
Lahart [39] | x | ||||||||||
Badger [68] | x | ||||||||||
Giese-Davis [60] | x | ||||||||||
Gnagnarella [47] | x | ||||||||||
Author | Outcomes | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Physical activity | Diet | Weight loss | HRQoL | Anxiety and depression symptoms | Shoulder mobility, wound healing | Occupational outcome | Self-efficacy | Emotional function | Sexual functioning | Fatigue | Social support, | Psychological well-being | Adaptive coping | Physical function | |
Gellert [73] | x | x | |||||||||||||
Marchioro [74] | x | x | x | x | x | ||||||||||
Marcus [63] | x | x | x | x | |||||||||||
Darga [40] | x | ||||||||||||||
Andersen [84] | x | x | |||||||||||||
Badger [69] | x | x | x | ||||||||||||
Badger [70] | x | ||||||||||||||
Badger [70] | x | x | x | x | |||||||||||
Giese-Davis [61] | x | x | x | x | |||||||||||
Maeda [78] | x | x | x | x | |||||||||||
Demark-Wahnefried [45] | x | x | x | x | |||||||||||
Sharif (2009) | x | x | x | x | |||||||||||
Hoving [79] | x | x | x | ||||||||||||
Marcus [64] | x | x | x | ||||||||||||
Lee [75] | x | ||||||||||||||
David [72] | x | x | |||||||||||||
Gonçalves [76] | x | x | x | x | x | x | |||||||||
Naumann [49] | x | ||||||||||||||
De Boer [80] | x | ||||||||||||||
Kim [66] | x | x | x | x | x | x | |||||||||
Spector [48] | x | x | |||||||||||||
Befort [43] | x | x | x | x | |||||||||||
McCarroll [25] | x | x | x | ||||||||||||
Badger [37] | x | ||||||||||||||
Arving [77] | x | x | x | x | |||||||||||
Carayol [46] | x | x | x | x | |||||||||||
Casla [51] | x | x | x | ||||||||||||
Cho [41] | x | ||||||||||||||
Demark-Wahnefried [52] | x | ||||||||||||||
Rogers [53] | x | x | |||||||||||||
Loh [58] | x | x | x | ||||||||||||
Lahart [39] | x | x | x | ||||||||||||
Badger [37] | x | ||||||||||||||
Giese-Davis [60] | x | x | x | x | x | ||||||||||
Gnagnarella [47] | x | x | |||||||||||||
Rights and permissions
About this article
Cite this article
D’Egidio, V., Sestili, C., Mancino, M. et al. Counseling interventions delivered in women with breast cancer to improve health-related quality of life: a systematic review. Qual Life Res 26, 2573–2592 (2017). https://doi.org/10.1007/s11136-017-1613-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-017-1613-6