Abstract
Background
Intradural spinal metastases are rare, and little is known regarding surgical indications and outcomes.
Methods
A retrospective search identified adults with intradural spinal metastases operated on at the Mayo Clinic from 1994-2011. Data were collected regarding demographics, tumor type and location, and outcomes.
Results
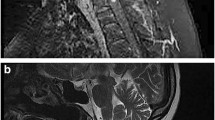
Fifteen patients with intradural spinal metastases were investigated. The age range was 38-74 years (mean = 55 years; ±SD = 11.1). Predominant tumor location and type were lumbosacral and adenocarcinoma, respectively: 3 intramedullary and 12 extramedullary. Patients were operated on to relieve or prevent progressive/intractable neurological sequelae and/or pain. Of 13 who underwent resection, gross total removal was reported in 10; simple biopsy was performed in 2. There was one surgical complication, no medical complications, and no surgical mortality. At median follow-up of 1 month postoperatively, 10 of 15 patients were stable or improved. Of 13 patients who underwent resection, 10 were stable or improved. Of two patients who underwent biopsy, neither was stable or improved at follow-up. Using the Modified McCormick Scale, 11 of 15 patients were “functional” preoperatively and 4 went from “functional” preoperatively to “non-functional” postoperatively. Three of those four died within 60 days of surgery from systemic disease progression. Median hospital stay was 8 days. Ten of 15 patients died by the end of the study period, and the median survival of 15 patients was 5 months.
Conclusions
With improved outcomes in metastatic cancer, more patients are encountered in practice. An aggressive surgical approach is warranted for extramedullary lesions, whereas caution is advised for intramedullary lesions. Postoperative functional decline is more likely due to systemic disease progression rather than surgery.



Similar content being viewed by others
Abbreviations
- MMS:
-
Modified McCormick Scale
References
Bartels RH, Feuth T, van der Maazen R, Verbeek AL, Kappelle AC, André Grotenhuis J, Leer JW (2007) Development of a model with which to predict the life expectancy of patients with spinal epidural metastasis. Cancer 110(9):2042–2049
Bartels RH, van der Linden YM, van der Graaf WT (2008) Spinal extradural metastasis: review of current treatment options. CA Cancer J Clin 58(4):245–259
Chow TS, McCutcheon IE (1996) The surgical treatment of metastatic spinal tumors within the intradural extramedullary compartment. J Neurosurg 85:225–230
Cole JS, Patchell RA (2008) Metastatic epidural spinal cord compression. Lancet Neurol 7(5):459–466
Fornasier VL, Horne JG (1975) Metastases to the vertebral column. Cancer 36:590–594
Frey I, Le Breton C, Lefkopoulos A, Perrot N, Khalil A, Chopier J, Le Blanche A, Bigot JM (1998) Intradural extramedullary spinal canal secondary neoplasms: MR findings in 30 patients. Eur Radiol 8:1187–1192
Grant R, Papadopoulos SM, Greenberg HS (1991) Metastatic epidural spinal cord compression. Neurol Clin 9:825–841
Harel R, Angelov L (2010) Spine metastases: current treatments and future directions. Eur J Cancer 46(15):2696–2707
Kim DY, Lee JK, Moon SJ, Kim SC, Kim CS (2009) Intradural spinal metastasis to the cauda equina in renal cell carcinoma: a case report and review of the literature. Spine 34(24):892–895
Loblaw DA, Laperriere NJ, Mackillop WJ (2003) A population-based study of malignant spinal cord compression in Ontario. Clin Oncol (R Coll Radiol) 15(4):211–217
McCormick PC, Torres R, Post KD (1990) Intramedullary ependymoma of the spinal cord. J Neurosurg 72:523–532
Mosdal C, Bang F (1981) Intradural spinal metastases. Acta Neurochir (Wien) 56:107–110
Perrin RG, Livingston KE, Aarabi B (1982) Intradural extramedullary spinal metastasis. a report of 10 cases. J Neurosurg 56(6):835–837
Schick U, Marquardt G, Lorenz R (2001) Intradural and extradural spinal metastases. Neurosurg Rev 24(1):1–5 [discussion 6–7]
Tognetti F, Lanzino G, Calbucci F (1988) Metastases of the spinal cord from remote neoplasms. study of five cases. Surg Neurol 30(3):220–227
van der Linden YM, Dijkstra SP, Vonk EJ, Marijnen CA, Leer JW (2005) Prediction of survival in patients with metastases in the spinal column: results based on a randomized trial of radiotherapy. Cancer 103(2):320–328
Acknowledgments
Conflicts of interest
None.
Disclosures
No financial disclosures
Disclosure of funding
Non-funded
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Spinal intradural metastases are a growing medical problem; accordingly, publications on the topic are welcomed. A recent paper (October 2011) published in Acta Neurochirurgica on the same subject, harboring a similar number of patients, displayed similar conclusions. The conclusions presented in this paper should be regarded with caution, as this is a highly selected population of surgical patients, and indications for surgery were not clear, in comparison with non-operated patients featuring the same disease.
No doubt, I can see an interest in surgery of spinal intradural metastasis in order to obtain a histopathological diagnosis, to decompress neural elements and increase functional capability, and to relieve pain. However, in this paper there is little data presentation or discussion about the systemic staging of the primary disease, which for me is a key element in the surgical treatment decision. Patients who have a short mean survival after a surgical procedure (5 months as the mean survival rate, and 2 months for non-functional preoperative patients) probably shouldn't be operated on as it comprises an inappropriate use of resources, despite the low complication rate (7%) or the short length of stay (8 days). A pertinent fact, as the authors showed, is that the percentage of functional patients decreased with surgery from 73% to 53%, despite only one patient going from functional to non-functional.
Nevertheless, the authors present interesting data on the epidemiology, location, and natural history of surgically treated patients harboring spinal intradural metastasis. It seems that intramedullary tumors have worse outcomes, and of course biopsy is not a successful form of treatment.
In the strict sense, I don't fully agree with the authors' statement that "an aggressive approach is warranted for extramedullary lesions, whereas caution is advised for intramedullary ones." Even for extramedullary lesions the decision to treat surgically depends on the extent of primary disease and on the systemic disease progression. The key element is systemic oncologic stating and consequent life expectancy. In this perspective, their management isn't different from that for spinal extradural metastases.
Oscar Alves
Porto, Portugal
Rights and permissions
About this article
Cite this article
Hoover, J.M., Krauss, W.E. & Lanzino, G. Intradural spinal metastases: a surgical series of 15 patients. Acta Neurochir 154, 871–877 (2012). https://doi.org/10.1007/s00701-012-1313-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-012-1313-5