Abstract
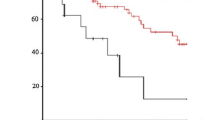
We investigated the relationship between postoperative complications and prognosis in esophageal cancer patients. Two hundred five patients with esophageal cancer were divided into three case groups. Group A (n = 100) consisted of cases without postoperative complications. Groups B (n = 58) and C (n = 47) consisted of cases with minor and major postoperative complications. The 5-year survival rates were 41.8%, 21.3%, and 20.2% in groups A, B, and C, respectively. There was a significant difference in the prognosis between groups A and B, and also between groups A and C. Any patients who died within 5 years without a relapse their cases were excluded from the study; the 5-year survival rates were 46.7%, 32.3%, and 22.5% in groups A, B, and C, respectively, with a significant difference between groups A and B. There were no significant differences between the three groups regarding the patient characteristics. These results therefore indicate that postoperative complications might contribute to a poor prognosis in cancer patients.
Similar content being viewed by others
References
Hafstrom L, Holmin T (1978) Relatioship between postoperative temperature and survival in patients resected for colorectal cancer. Am J Surg 135:312–314
Liechty RD, Vanourny SE, Ziffren SE (1968) Intraperitoneal infection and cancer of the colon and rectum. Arch Surg 96:599–603
Nowacki MP, Szymendera JJ (1983) The strongest prognostic factors in colorectal carcinoma. Dis Colon Rectum 26:263–268
DerHagopian RP, Sugarbaker EV, Ketcham A (1978) Inflammatory oncotaxis. JAMA 240:374–375
Yamaguchi Y, Toge T (1996) The immunological response of SIRS patients (in Japanese). Surg Trauma Immunol Responses 5:19–21
Hattori T, Hamai Y, Takiyama W, Hirai T, Ikeda T (1980) Enhancing effect of thoracotomy on tumor growth in rats with special reference to the duration and timing of the operation. Gann (Cancer) 71:280–284
Hirai T, Yoshimoto A, Iwata T, Yamashita Y, Kuwahara M, Toge T (1997) Enhancing effect of thoraco-laparotomy on liver metastasis and the role played by active oxygens in its mechanism. Surg Today 27:1040–1045
Jackson RM, Rice DH (1990) Wound infections and recurrence in head and neck cancer. Otolaryngol Head Neck Surg 102:331–333
Grandis JR, Snyderman CH, Johnson JT, Yu VL, D’Amico F (1992) Postoperative wound infection. Cancer 70:2166–2170
Sensenig DM, Rossi NP, Ehrenhaft JL (1963) Results of the surgical treatment of bronchogenic carinoma. Surg Gynecol Obstet 116:279–284
Ruckdeschel JC, Codish SD, Stranahan A, Mackneally MF (1972) Post-operative empyema improves survival in lung cancer. N Engl J Med 287:1013–1017
Weissmann G, Smolen JE, Korchak HM (1980) Release of inflammatory mediators from stimulated neutrophils. N Engl J Med 303:27–34
Babior BM, Kipnes RS, Curnutte JT (1973) Biological defense mechanisms: the production by leukocytes of superoxide, a potential bactericidal agent. J Clin Invest 52:741–744
Orr FW, Adamson IYR, Warner D, Leroyer V, Werner L, Shaughnessey S, Young L (1988) The effect of oxygen radicalmediated pulmonary endothelial damage on cancer metastasis. Mol Cell Biochem 84:189–198
Orr FW, Warner DJA (1987) Effects of neutrophil-mediated pulmonary endothelial injury on the localization and metastasis of circulating Walker carcinosarcoma cells. Invas Metast 7:183–196
Weiss SJ, Young J, Lobuglio AF, Slivka A, Nimen N (1981) Role of hydrogen peroxide in neutrophil-mediated destruction of cultured endothelial cells. J Clin Invest 68:714–721
Van Zee KJ, Deforge LE, Fisher E, Marano MA, Kenny JS, Remick DG, Lowry SF, Moldawer LL (1991) IL-8 in septic shock, endotoxemia, and after IL-1 administration. J Immunol 146:3478–3482
Sakamoto K, Arakawa H, Mita S, Ishiko T, Ikei S, Egami H, Hisano S, Ogawa M (1994) Elevation of circulating Interleukin 6 after surgery: factors influencing the serum level. Cytokine 6:181–186
Bevilacqua MP, Pober JS, Wheeler ME, Cotran RS, Gimbrone MA Jr (1985) Interleukin 1 acts on cultured human vascular endothelium to increase the adhesion of polymorphonuclear leukocytes, monocytes, and related leukocyte cell lines. J Clin Invest 76:2003–2001
Ogawa M (1994) Activation of neutrophils by cytokines is closely related to the development of organ dysfunction (in Japanese). Igaku No Ayumi 169:845–849
Sameshima H, Ikei S, Mori K, Yamaguchi Y, Egami H, Misumi M, Moriyasu M, Ogawa M (1993) The role of tumor necrosis factor-α in the aggravation of cerulein-induced pancreatitis in rats. Int J Pancreatol 14:107–115
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Hirai, T., Yamashita, Y., Mukaida, H. et al. Poor prognosis in esophageal cancer patients with postoperative complications. Surg Today 28, 576–579 (1998). https://doi.org/10.1007/s005950050187
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/s005950050187