Abstract
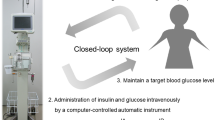
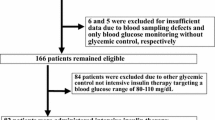
Van den Berghe et al. reported in 2001 that tight glycemic control (maintaining blood glucose levels at 80–110 mg/dl) improved morbidity and mortality in the surgical intensive care unit. This method was termed intensive insulin therapy (IIT), and it is now being adopted worldwide for perioperative care. Recent evidence has suggested that perioperative hyperglycemia significantly contributes to the development of postoperative infection (POI). Many professional societies therefore now recommend IIT over conventional standard glycemic control measures for critically ill adult patients to minimize infectious complications. However, IIT carries a risk of inducing hypoglycemia, which is linked to serious neurological events. We recently demonstrated that achieving perioperative tight glycemic control using an artificial endocrine pancreas for surgical patients was a safe and effective method for decreasing the incidence of POI without increasing the risk of hypoglycemia. We herein review the benefits and requirements of tight glycemic control in surgery, with a focus on infection control. Strict perioperative glycemic control using a closed-loop artificial endocrine pancreas system is recommended for safe and effective performance of IIT.
Similar content being viewed by others
References
Van den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M, et al. Intensive insulin therapy in critically ill patients. N Engl J Med 2001;345:1359–1367.
Van den Berghe G, Wilmer A, Hermans G, Meersseman W, Wouters PJ, Milants I, et al. Intensive insulin therapy in the medical ICU. N Engl J Med 2006;354:449–461.
Krinsley JS. Effects of an intensive glucose management protocol on the mortality of critically ill adult patients. Mayo Clin Proc 2004;79:992–1000.
Klein D, Schubert T, Horch RE, Jauch KW, Jeschke MG. Insulin treatment improves hepatic morphology and function through modulation of hepatic signals after severe trauma. Ann Surg 2004;240:340–349.
McMullin J, Brozek J, Jaeschke R, Hamielec C, Dhingra V, Rocker G, et al. Glycemic control in the ICU: a multicenter survey. Intensive Care Med 2004;30:798–803.
Kanji S, Buffie J, Hutton B, Bunting PS, Singh A, McDonald K, et al. Reliability of point-of-care testing for glucose measurement in critically ill adults. Crit Care Med 2005;33:2778–2785.
Schultz MJ, Spronk P, Moeniralam H. Tight glycemic control: a survey of intensive care practice in the Netherlands. Intensive Care Med 2006;32:618–619.
Vriesendorp TM, DeVries JH, van Santen S, Moeniralam HS, de Jonge E, Roos YB, et al. Evaluation of short-term consequences of hypoglycemia in an intensive care unit. Crit Care Med 2006;34:2714–2718.
Krinsley JS, Jones RL. Cost analysis of intensive glycemic control in critically ill adult patients. Chest 2006;129:644–650.
Mitchell I, Finfer S, Bellomo R, Higlett T; Anzics Clinical Trials Group Glucose Management Investigators. Management of blood glucose in the critically ill in Australia and New Zealand: a practice survey and inception cohort study. Intensive Care Med 2006;32:867–874.
Van den Berghe G, Schoonheydt K, Becx P, Bruyninckx F, Wouters PJ. Insulin therapy protects the central and peripheral nervous system of intensive care patients. Neurology 2005;64:1348–1353.
Van den Berghe G, Wouters PJ, Kesteloot K, Hilleman DE. Analysis of healthcare resource utilization with intensive insulin therapy in critically ill patients. Crit Care Med 2006;34:612–616.
Ramos M, Khaipey Z, Lipsitz S, Steinberg J, Panizales MT, Zinner M, et al. Relationship of perioperative hyperglycemia and postoperative infections in patients who undergo general and vascular surgery. Ann Surg 2008;248:585–591.
Ambiru S, Kato A, Kimura F, Shimizu H, Yoshidome H, Otsuka M, et al. Poor postoperative blood glucose control increases surgical site infections after surgery for hepato-biliary-pancreatic cancer: a prospective study in a high-volume institute in Japan. J Hosp Infect 2008;68:230–233.
Van den Berghe G. Insulin therapy in the intensive care unit should be targeted to maintain blood glucose between 4.4 mmol/l and 6.1 mmol/l. Diabetologia 2008;51:911–915.
Fietsam R Jr, Bassett J, Glover JL. Complications of coronary artery surgery in diabetic patients. Ann Surg 1991;57:551–557.
O’Neill PA, Davies I, Fullerton KJ, Bennett D. Stress hormone and blood glucose response following acute stroke in the elderly. Stroke 1991;22:842–847.
Scott JF, Robinson GM, French JM, O’Connell JE, Alberti KG, Gray CS. Glucose potassium insulin infusions in the treatment of acute stroke patients with mild to moderate hyperglycemia: the glucose insulin in stroke trial (GIST). Stroke 1999;30:793–799.
McManus LM, Bllodworth RC, Prihoda TJ, Blodgett JL, Pinckard RN. Agonist-dependent failure of neutrophil function in diabetes correlates with extent of hyperglycemia. J Leukoc Biol 2001;70:395–404.
Van den Berghe G, Wouters PJ, Bouillon R, Weekers F, Verwaest C, Schetz M, et al. Outcome benefit of intensive insulin therapy in the critically ill: insulin dose versus glycemic control. Crit Care Med 2003;31:359–366.
Dellinger RP, Levy M, Cartlet J, Bion J, Parker MM, Jaeschke R, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock. Intensive Care Med 2008;34:17–60.
Runkhorst FM, Engel C, Bloos F, Meier-Hellmann A, Ragaller M, Weiler N, et al.: German Competence Network Sepsis (SepNet). Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N Engl J Med 2008;358:125–139.
National Institutes of Health. Glucontrol study. Comparing the effects of two glucose control regimens by insulin in intensive care unit patients. ClinicalTrials.gov identifier: NCT 00107601.
NICE-SUGAR Study Investigators, Finfer S, Chittock DR, Su SY, Blair D, Foster D, Dhingra V, et al. Intensive versus conventional glucose control in critically ill patients. N Engl J Med 2009;360:1283–1297.
Wiener RS, Wiener DC, Larson RJ. Benefits and risks of tight glucose control in critically ill adults. JAMA 2008;300:933–944.
Billota F, Spinelli A, Giovannini F, Doronzio A, Edlfini R, Rosa G. The effect of intensive insulin therapy on infection rate, vasospasm, neurologic outcome, and mortality in neurointensive care unit after intracranial aneurysm clipping in patients with acute subarachnoid hemorrhage: a randomized prospective pilot trial. J Neurosurg Anesthesiol 2007;19:156–160.
Aljada A, Ghanim H, Mohanty P, Kapur N, Dandona P. Insulin inhibits the pro-inflammatory transcription factor early growth response gene-1 (Egr)-1 expression in mononuclear cells (MNC) and reduces plasma tissue factor (TF) and plasminogen activator inhibitor-1 (PAI-1) concentrations. J Clin Endocrinol Metab 2002;87:1419–1422.
Dandona P, Aljada A, Mohanty P, Ghanim H, Hamouda W, Assian E, et al. Insulin inhibits intranuclear nuclear factor κB and stimulates iκB in mononuclear cells in obese subjects: evidence for an anti-inflammatory effect? J Clin Endocrinol Metab 2001;86:3257–3265
Aljada A, Ghanim H, Mohanty P, Syed T, Bandyopadhyay A, Dandona P. Glucose intake induces an increase in activator protein 1 and early growth response 1 binding activities, in the expression of tissue factor and matrix metalloproteinase in mononuclear cells, and in plasma tissue factor and matrix metalloproteinase concentrations. Am J Clin Nutr 2004;80:51–57.
Iwasaka H. Anti-inflammatory effects of insulin (abstract in English). ICU & CCU 2008;32:821–831.
Hanazaki K, Nosé Y, Brunicardi FC. Artificial endocrine pancreas: a review. J Am Coll Surg 2001;193:310–322.
Yamashita K, Okabayashi T, Yokoyama T, Yatabe T, Maeda H, Manabe M, et al. The accuracy of a continuous blood glucose monitor during surgery. Anesth Analg 2008;106(1):160–163.
Yamashita K, Okabayashi T, Yokoyama T, Yatabe T, Maeda H, Manabe M, et al. Accuracy and reliability of continuous blood glucose monitoring in post-surgical patients. Acta Anaesthesiol Scand 2009;53(1):66–71.
Okabayashi T, Hanazaki K, Nishimori I, Sugimoto T, Maeda H, Yatabe T, et al. Continuous post-operative blood monitoring and control using a closed-loop system in patients undergoing hepatic resection. Dig Dis Sci 2008;53:1405–1410.
Kono T, Hanazaki K, Yazawa K, Ashizawa S, Fisher WE, Wang XP, et al. Pancreatic polypeptide administration reduces insulin requirements of artificial pancreas in pancreatectomized dogs. Artif Organs 2005;29:83–87.
Zerr KJ, Furnary AP, Grunkemeier GL, Bookin S, Kanhere V, Starr A. Glucose control lowers the risk of wound infection in diabetes after open heart operations. Ann Thorac Surg 1997;63:356–361.
Furnary AP, Zerr KJ, Grunkemeier GL, Starr A. Continuous intravenous insulin infusion reduces the incidence of deep sternal wound infection in diabetic patients after cardiac surgical procedures. Ann Throc Surg 1999;67:352–362.
Okabayashi T, Nishimori I, Yamashita K, Sugimoto T, Maeda H, Yatabe T, et al. Continuous postoperative blood glucose monitoring and control by an artificial pancreas in patients undergoing pancreatic resection: a prospective randomized clinical trial. Arch Surg 2009;144:933–937.
Okabayashi T, Nishimori I, Maeda H, Yamashita K, Yatabe T, Hanazaki K. Effect of intensive insulin therapy using a closed-loop glycemic control system in hepatic resection patients: a prospective randomized clinical trial. Diabetes Care 2009;32:1425–1427.
Rafoth RJ. Standardizing sliding scale insulin orders. Am J Med Qual 2002;17:175–178.
Hanazaki K, Okabayashi T, Maeda H. Tight glycemic control using an artificial pancreas to control perioperative hyperglycemia decreases surgical site infection in pancreatectomized or hepatectomozied patients. Ann Surg 2009;250:351–352.
Hanazaki K, Okabayashi T, Maeda H, Kitagawa H, Sugimoto T, Yatabe T, et al. Perioperative blood glucose control using artificial endocrine pancreas (abstract in English). ICU & CCU 2008;32:805–813.
Hanazaki K, Okabayashi T, Maeda H, Yatabe T, Yamashita K, Nishimori I, et al. Perioperative blood glucose control using artificial endocrine pancreas-Importance of perioperative strict glycemic control (in Japanese). Tan & Sui 2008;29:861–866.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Hanazaki, K., Maeda, H. & Okabayashi, T. Tight perioperative glycemic control using an artificial endocrine pancreas. Surg Today 40, 1–7 (2010). https://doi.org/10.1007/s00595-009-4061-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-009-4061-2