Abstract
Background
The aim of this study was to validate the safety and feasibility of pure laparoscopic extended cholecystectomy (LEC) by comparing the outcome with that of open extended cholecystectomy (OEC). Moreover, on the basis of our experience, we also aimed to investigate the learning curve of pure LEC.
Methods
This single-center study enrolled patients who were diagnosed primary gallbladder cancer with pathologically confirmed and underwent R0 resection with curative intent between January 2016 and December 2019. A total of 31 patients who underwent OEC and 17 patients who underwent LEC were selected. Propensity score matching analysis was performed in a 1:1 ratio using the nearest-neighbor matching method, and clinical information was retrospectively collected from medical records and analyzed.
Results
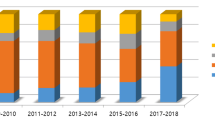
The postoperative hospital stay was statistically shorter in the LEC group (7 days) than in the OEC group (12 days). The overall surgical complication rate did not differ between the two groups. The 1- and 3-year disease-free survival rates were 82.4% and 82.4% in the OEC group and 94.2% and 71.5% in the LEC group, respectively (P = 0.94). Considering the correlation between the number of cumulative cases and the operation time and between the number of cumulative cases and the number of retrieved lymph nodes in the LEC group, as the cases were accumulated, both the operation time and the number of retrieved lymph nodes had a statistically significant correlation with the number of cases.
Conclusions
LEC showed a significant advantage in terms of achieving shorter postoperative hospital stay and similar results to OEC with respect to overall complications and pathological outcomes. The present results confirm that laparoscopy can be considered a safe treatment for primary gallbladder cancer in selected patients.



Similar content being viewed by others
References
Benoist S, Panis Y, Fagniez PL (1998) Long-term results after curative resection for carcinoma of the gallbladder. French University Association for Surgical Research. Am J Surg 175:118–122
Duffy A, Capanu M, Abou-Alfa GK et al (2008) Gallbladder cancer (GBC): 10-year experience at Memorial Sloan-Kettering Cancer Centre (MSKCC). J Surg Oncol 98:485–489
Goetze TO (2015) Gallbladder carcinoma: prognostic factors and therapeutic options. World J Gastroenterol 21:12211–12217
Choi KS, Choi SB, Park P et al (2015) Clinical characteristics of incidental or unsuspected gallbladder cancers diagnosed during or after cholecystectomy: a systematic review and meta-analysis. World J Gastroenterol 21:1315–1323
Kim HS, Park JW, Kim H et al (2018) Optimal surgical treatment in patients with T1b gallbladder cancer: an international multicenter study. J Hepatobiliary Pancreat Sci 25:533–543
Yoon YS, Han HS, Cho JY et al (2015) Is laparoscopy contraindicated for gallbladder cancer? A 10-year prospective cohort study. J Am Coll Surg 221:847–853
Shih SP, Schulick RD, Cameron JL et al (2007) Gallbladder cancer: the role of laparoscopy and radical resection. Ann Surg 245:893–901
Castro CM, Santibañez SP, Rivas TC et al (2018) Totally laparoscopic radical resection of gallbladder cancer: technical aspects and long-term results. World J Surg 42:2592–2598
Han HS, Yoon YS, Agarwal AK et al (2019) Laparoscopic surgery for gallbladder cancer: an expert consensus statement. Dig Surg 36:1–6
Nag HH, Sachan A, Nekarakanti PK (2019) Laparoscopic versus open extended cholecystectomy with bi-segmentectomy (s4b and s5) in patients with gallbladder cancer. J Minim Access Surg. https://doi.org/10.4103/jmas.jmas_98_19
Gumbs AA, Hoffman JP (2010) Laparoscopic radical cholecystectomy and Roux-en-Y choledochojejunostomy for gallbladder cancer. Surg Endosc 24:1766–1768
Whalen GF, Bird I, Tanski W et al (2001) Laparoscopic cholecystectomy does not demonstrably decrease survival of patients with serendipitously treated gallbladder cancer. J Am Coll Surg 192:189–195
Kasumova GG, Tabatabaie O, Najarian RM et al (2017) Surgical management of gallbladder cancer: simple versus extended cholecystectomy and the role of adjuvant therapy. Ann Surg 266:625–631
Berger-Richardson D, Chesney TR, Englesakis M et al (2017) Trends in port-site metastasis after laparoscopic resection of incidental gallbladder cancer: a systematic review. Surgery 161:618–627
Lundberg O, Kristoffersson A (1999) Port site metastases from gallbladder cancer after laparoscopic cholecystectomy. Results of a Swedish survey and review of published reports. Eur J Surg 165:215–222
Z’Graggen K, Birrer S, Maurer CA et al (1998) Incidence of port site recurrence after laparoscopic cholecystectomy for preoperatively unsuspected gallbladder carcinoma. Surgery 124:831–838
Cherqui D, Soubrane O, Husson E et al (2002) Laparoscopic living donor hepatectomy for liver transplantation in children. Lancet 359:392–396
Kim WJ, Kim KH, Kim SH et al (2018) Laparoscopic versus open liver resection for centrally located hepatocellular carcinoma in patients with cirrhosis: a propensity score-matching analysis. Surg Laparosc Endosc Percutan Tech 28:394–400
Soubrane O, de Rougemont O, Kim KH et al (2015) Laparoscopic living donor left lateral sectionectomy: a new standard practice for donor hepatectomy. Ann Surg 262:757–761 (discussion 761–763)
Piccolo G, Ratti F, Cipriani F et al (2019) Totally laparoscopic radical cholecystectomy for gallbladder cancer: a single center experience. J Laparoendosc Adv Surg Tech A 29:741–746
Kim DH, Kim SH, Choi GH et al (2013) Role of cholecystectomy and lymph node dissection in patients with T2 gallbladder cancer. World J Surg 37:2635–2340
Shirobe T, Maruyama S (2015) Laparoscopic radical cholecystectomy with lymph node dissection for gallbladder carcinoma. Surg Endosc 29:2244–2250
Chijiiwa K, Noshiro H, Nakano K et al (2000) (2000) Role of surgery for gallbladder carcinoma with special reference to lymph node metastasis and stage using western and Japanese classification systems. World J Surg 24:1271–1276
Miyazaki M, Yoshitomi H, Miyakawa S et al (2015) Clinical practice guidelines for the management of biliary tract cancers 2015: the 2nd English edition. J Hepatobiliary Pancreat Sci 22:249–273
Wakabayashi H, Ishimura K, Hashimoto N et al (2004) Anlaysis of prognostic factors after surgery for stage III and IV gallbladder cancer. Eur J Surg Oncol 30(8):842–846
Acknowledgements
We would like to give special thanks to Mr. Dan-te An at Korea University Guro Hospital for his help in figure making.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Wan-Joon Kim, Tae-Wan Lim, Pyoung-Jae Park, Sae-Byeol Choi, and Wan-Bae Kim have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kim, WJ., Lim, TW., Park, PJ. et al. Safety and feasibility of pure laparoscopic extended cholecystectomy: comparison with the open technique in a propensity analysis at a single center. Surg Endosc 35, 6166–6172 (2021). https://doi.org/10.1007/s00464-020-08112-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-08112-3