Abstract
Background
Animal experiments have suggested that the laparoscopic peritoneal environment is hypoxic. This study aimed to investigate whether peritoneal tissue is hypoxic on a cellular level during a carbon dioxide (CO2) pneumoperitoneum at different intraperitoneal pressures (IPPs) and to determine the short-term effects of surgical injury on the hypoxia status of peritoneal tissue in the injured peritoneum and the distant noninjured peritoneum at cellular and molecular levels.
Methods
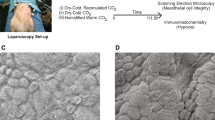
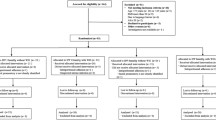
Experiment 1: Mice were divided into five groups according to the following treatments: anesthesia alone, laparotomy, and CO2 pneumoperitoneum at IPPs of 2, 8, or 15 mmHg. Over the course of each experiment, the peritoneal tissue-oxygen tension (PitO2) was continuously monitored. Experiment 2: On the first day, the mice were divided into three groups according to the following treatments: CO2 pneumoperitoneum at an IPP of either 2 or 8 mmHg or laparotomy. The bilateral caudal epigastric arteries and uterine horns then were coagulated using a bipolar cautery device. On day 7, peritoneal tissue samples were collected for real-time reverse transcriptase–polymerase chain reaction (RT-PCR) and immunohistochemistry. In both experiments, pimonidazole hydrochloride was used to detect tissue hypoxia at a cellular level.
Results
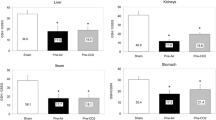
Experiment 1: Peritoneal hypoxia at both tissue and cellular levels was detected only in the groups treated with an IPP of 15 mmHg (PitO2: 5.2 ± 1.0 mmHg, mean ± SEM). Experiment 2: The percentage of pimonidazole immunostained mesothelial and stromal cells from the distant noninjured peritoneum was significantly higher in the group treated with an IPP of 8 mmHg than in the other groups. Hypoxia-inducible factor 1 alpha subunit mRNA expression in the distant noninjured peritoneum of the group treated with an IPP of 8 mmHg was significantly higher than in the control group (anesthesia alone).
Conclusion
The CO2 pneumoperitoneum itself did not cause peritoneal hypoxia at either a tissue or a cellular level in a mouse model when a low IPP was used.






Similar content being viewed by others
References
Ray NF, Denton WG, Thamer M, Henderson SC, Perry S (1998) Abdominal adhesiolysis: in patient care and expenditures in the United Stares in 1994. J Am Coll Surg 186:1–9
Yesildaglar N, Koninckx PR (2000) Adhesion formation in intubated rabbits increases with high insufflation pressure during endoscopic surgery. Hum Reprod 15:687–691
Molinas CR, Koninckx PR (2000) Hypoxaemia induced by CO2 or helium pneumoperitoneum is a cofactor in adhesion formation in rabbits. Hum Reprod 15:1758–1763
Molinas CR, Mynbaev O, Pauwels A, Novak P, Koninckx PR (2001) Peritoneal mesothelial hypoxia during pneumoperitoneum is a cofactor in adhesion formation in a laparoscopic mouse model. Fertil Steril 76:560–567
Mynbaev OA, Molinas CR, Adamyan LV, Vanacker B, Koninckx PR (2002) Reduction of CO2-pneumoperitoneum-induced metabolic hypoxaemia by the addition of small amounts of O2 to the CO2 in a rabbit ventilated model: a preliminary study. Hum Reprod 17:1623–1629
Binda MM, Molinas CR, Koninckx PR (2003) Reactive oxygen species and adhesion formation: clinical implications in adhesion prevention. Hum Reprod 18:2503–2507
Wildbrett P, Oh A, Naundorf D, Volk T, Jacobi CA (2003) Impact of laparoscopic gases on peritoneal microenvironment and essential parameters of cell function. Surg Endosc 17:78–82
Elkelani OA, Binda MM, Molinas CR, Koninckx PR (2004) Effect of adding more than 3% oxygen to carbon dioxide pneumoperitoneum on adhesion formation in a laparoscopic mouse model. Fertil Steril 82:1616–1622
Molinas CR, Tjwa M, Vanacker B, Binda MM, Elkelani O, Koninckx PR (2004) Role of CO2-pneumoperitoneum-induced acidosis in CO2 pneumoperitoneum-enhanced adhesion formation in mice. Fertil Steril 81:708–711
Crowther M, Brown NJ, Bishop ET, Lewis CE (2001) Microenvironmental influence on macrophage regulation of angiogenesis in wounds and malignant tumors. J Leukoc Biol 70:478–490
Murdoch C, Giannoudis A, Lewis CE (2004) Mechanisms regulating the recruitment of macrophages into hypoxic areas of tumors and other ischemic tissues. Blood 104:2224–2234
Lewis C, Murdoch C (2005) Macrophage responses to hypoxia: implications for tumor progression and anticancer therapies. Am J Pathol 167:627–635
Bourdel N, Matsuzaki S, Bazin JE, Pouly JL, Mage G, Canis M (2007) Peritoneal tissue-oxygen tension during a carbon dioxide pneumoperitoneum in a mouse laparoscopic model with controlled respiratory support. Hum Reprod 22:1149–1155
Mynbaev OA, Corona R (2009) Possible mechanisms of peritoneal tissue-oxygen tension changes during CO2 pneumoperitoneum: the role of design, methodology, and animal models. Hum Reprod 24:1242–1246
Akca O, Melischek M, Scheck T, Hellwagner K, Arkilic CF, Kurz A et al (1999) Postoperative pain and subcutaneous oxygen tension. Lancet 354:41–42
Greif R, Akca O, Horn EP, Kurz A, Sessler DI (2000) Supplemental perioperative oxygen to reduce the incidence of surgical-wound infection. Outcomes research group. N Engl J Med 342:161–167
Matsuzaki S, Canis M, Bazin JE, Darcha C, Pouly JL, Mage G (2007) Effects of supplemental perioperative oxygen on postoperative abdominal wound adhesions in a mouse laparotomy model with controlled respiratory support. Hum Reprod 22:2702–2706
Bourdel N, Matsuzaki S, Bazin JE, Darcha C, Pouly JL, Mage G, Canis M (2008) Postoperative peritoneal dissemination is not promoted by carbon dioxide pneumoperitoneum at low intraperitoneal pressure in a mouse laparoscopic model with controlled respiratory support. J Minim Invasive Gynecol 15:321–326
Matsuzaki S, Bourdel N, Darcha C, Dechelotte PJ, Bazin JE, Pouly JL, Mage G, Canis M (2009) Molecular mechanisms underlying postoperative peritoneal dissemination might differ between a laparotomy and CO2 pneumoperitoneum: a syngeneic mouse model with controlled respiratory support. Surg Endosc 23:705–714
Matsuzaki S, Azuar AS, Mage G, Canis M (2009) Impact of the surgical peritoneal environment on preimplanted tumors on a molecular level: a syngeneic mouse model. J Surg Res (in press)
Azuar AS, Matsuzaki S, Darcha C, Dechelotte PJ, Pouly JL, Mage G, Canis M (2009) Impact of the surgical peritoneal environment on postoperative tumor growth and dissemination in a preimplanted tumor model. Surg Endosc 231:1733–1739
U.S. Department of Health and Human Services, Public Health Service (1985) Guide for the care and use of laboratory animals. National Institutes of Health, Bethesda, MD. NIH publication no. 86-23, revised
Molinas CR, Elkelani O, Campo R, Luttun A, Carmeliet P, Koninckx PR (2003) Role of the plasminogen system in basal adhesion formation and carbon dioxide pneumoperitoneum-enhanced adhesion formation after laparoscopic surgery in transgenic mice. Fertil Steril 80:184–192
Molinas CR, Campo R, Elkelani OA, Binda MM, Carmeliet P, Koninckx PR (2003) Role of hypoxia-inducible factors 1 alpha and 2 alpha in basal adhesion formation and in carbon dioxide pneumoperitoneum-enhanced adhesion formation after laparoscopic surgery in transgenic mice. Fertil Steril 80(Suppl 2):795–802
Molinas CR, Binda MM, Carmeliet P, Koninckx PR (2004) Role of vascular endothelial growth factor receptor 1 in basal adhesion formation and in carbon dioxide pneumoperitoneum-enhanced adhesion formation after laparoscopic surgery in mice. Fertil Steril 82(Suppl 3):1149–1153
Sawada T, Tsukada K, Hasegawa K, Ohashi Y, Udagawa Y, Gomel V (2001) Cross-linked hyaluronidase hydrogel prevents adhesion formation and reformation in mouse uterine horn model. Hum Reprod 16:353–356
Rout UK, Diamond MP (2003) Role of plasminogen activators during healing after uterine serosal lesioning in the rat. Fertil Steril 79:138–145
Sulaiman H, Dawson L, Laurent GJ, Bellingan GJ, Herrick SE (2002) Role of plasminogen activators in peritoneal adhesion formation. Biochem Soc Trans 30:126–131
Aarons CB, Cohen PA, Gower A, Reed KL, Leeman SE, Stucchi AF, Becker JM (2007) Statins (HMG-CoA reductase inhibitors) decrease postoperative adhesions by increasing peritoneal fibrinolytic activity. Ann Surg 245:176–184
Gross MW, Karbach U, Groebe K, Franko AJ, Mueller-Klieser W (1995) Calibration of misonidazole labeling by simultaneous measurement of oxygen tension and labeling density in multicellular spheroids. Int J Cancer 61:567–573
Haroon ZA, Raleigh JA, Greenberg CS, Dewhirst MW (2000) Early wound healing exhibits cytokine surge without evidence of hypoxia. Ann Surg 23:137–147
Jankovic B, Aquino-Parsons C, Raleigh JA, Stanbridge EJ, Durand RE, Banath JP (2006) Comparison between pimonidazole binding, oxygen electrode measurements, and expression of endogenous hypoxia markers in cancer of the uterine cervix. Cytometry B Clin Cytom 70:45–55
Samoszuk MK, Walter J, Mechetner E (2004) Improved immunohistochemical method for detecting hypoxia gradients in mouse tissues and tumors. J Histochem Cytochem 52:837–839
Matsuzaki S, Canis M, Darcha C, Pouly JL, Dechelotte P, Mage G (2006) Expression of WT1 is downregulated in eutopic endometrium obtained during the mid-secretory phase from patients with endometriosis. Fertil Steril 86:554–558
Matsuzaki S, Canis M, Darcha C, Dechelotte PJ, Pouly JL, Mage G (2008) Effects of a protein kinase C inhibitor on the initial development of ectopic implants in a syngenic mouse model of endometriosis. Fertil Steril 89:206–211
Ben-Haim M, Rosenthal RJ (1999) Causes of arterial hypertension and splachnic ischemia during acute elevations in intraabdominal pressure with CO2 pneumoperitoneum: a complex central nervous system-mediated response. Int J Colorectal Dis 14:227–236
Gutt CN, Schmandra TC (1999) Portal venous flow during CO2 pneumoperitoneum in the rat. Surg Endos 13:902–905
Booker WM, French DM, Molano PA (1947) Further studies on the acute effects of intraabdominal pressure. Am J Physiol 149:92–98
Suematsu T, Hirabayashi Y, Siraishi N, Adachi Y, Kitamura H, Kitano S (2001) Morphology of the murine peritoneum after pneuoperitoneum vs. laparotomy. Surg Endosc 15:954–958
Acknowledgments
We are grateful to the anesthesiology staff at CHU Clermont-Ferrand for their invaluable discussions. We are indebted to all the staff at le Centre International de la Chirurgie Endoscopique (Clermont-Ferrand, France) and the technicians in the Department of Anatomie et cytologie pathologiques, CHU Clermont-Ferrand, Hôtel-Dieu, for technical support. We are indebted to Karl Storz Endoscopy & GmbH (Tuttlingen, Germany) for providing laparoscopic equipment and Organon (Paris, France) for providing vecuronium bromide. This study was supported in part by Karl Storz Endoscopy & GmbH (Tuttlingen, Germany) and le Conseil Régional d’Auvergne (Recherche et Innovation Technologique) (Clermont-Ferrand, France).
Disclosures
Sachiko Matsuzaki, Kris Jardon, Elodie Maleysson, Francis D’Arpiany; Michel Canis, Jean-Etienne Bazin and Gérard Mage have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Matsuzaki, S., Jardon, K., Maleysson, E. et al. Carbon dioxide pneumoperitoneum, intraperitoneal pressure, and peritoneal tissue hypoxia: a mouse study with controlled respiratory support. Surg Endosc 24, 2871–2880 (2010). https://doi.org/10.1007/s00464-010-1069-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-010-1069-z