Abstract
The purpose of this study was to determine the significance of variables such as duration of the procedure, type of breast tissue, number of passes, depth of the biopsies, underlying pathology, the operator performing the procedure, and their effect on women’s perception of pain and discomfort during stereotactic large-core needle breast biopsy. One hundred and fifty consecutive patients with a non-palpable suspicious mammographic lesions were included. Between three and nine 14-gauge breast passes were taken using a prone stereotactic table. Following the biopsy procedure, patients were asked to complete a questionnaire. There was no discomfort in lying on the prone table. There is no relation between type of breast lesion and pain, underlying pathology and pain and performing operator and pain. The type of breast tissue is correlated with pain experienced from biopsy (P = 0.0001). We found out that patients with dense breast tissue complain of more pain from biopsy than patients with more involution of breast tissue. The depth of the biopsy correlates with pain from biopsy (P = 0.0028). Deep lesions are more painful than superficial ones. There is a correlation between the number of passes and pain in the neck (P = 0.0188) and shoulder (P = 0.0366). The duration of the procedure is correlated with pain experienced in the neck (P = 0.0116) but not with pain experienced from biopsy.
Similar content being viewed by others
Introduction
Stereotactic or ultrasonographically guided breast biopsy with large-core needles is a widely accepted alternative to needle-guided surgical biopsy in the diagnosis of pathologic breast lesions [1]. The use of stereotactic large-core needle breast biopsy (SLCNBB) is increasing, because the frequency of inadequate specimens is lower than in fine-needle aspiration (FNA), and it requires a less invasive procedure than open biopsy. At the same time SLCNBB can provide a more definitive diagnosis [2].
There are many variables which could affect the amount of pain and discomfort experienced by the patient during biopsy, such as: duration of the procedure, type of breast tissue, underlying histology of the lesion, number of passes, depth of the biopsies and the operator performing the procedure [3].
This prospective study was designed to evaluate the significance of these variables and their effect on women’s perception of pain and discomfort during SLCNBB.
Materials and methods
One hundred and fifty consecutive patients, from out patients clinic, with a non-palpable suspicious mammographic lesion were included in this study. There were no exclusion criteria. Mean age is 57.6 years (range: 32.1–84.9). During a time span of 16 months all 150 patients were included.
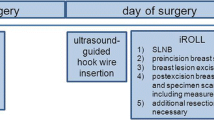
Biopsies were taken using a prone stereotactic table (Lorad stereoguide; Hologic, Bedford, Mass., USA,) after local anesthesia with 5 ml lidocaine. Lesions were localised with use of a digital detector, included in the stereotactic table.
Radiological characteristics of the lesions were classified as microcalcifictions (97), masses (38) and masses with calcification (15).
The number of passes varied from three to nine. The depth of the biopsy varied from 11.6 mm to 63.8 mm. Depth (z-axis) of the lesion was calculated by the Lorad stereoguide computer. The diameter of the lesions had an average of 8 mm. We did not have to use clips because there was no total removal of the lesions.
We used a 14-gauge core needle, long throw (22 mm excursion) automated biopsy device with multiple passes (Biopsygun; C.R. Bard, Covington, Ga., USA). We used specially trained radiographers (five, all female) and radiologists (five, one female and four male) for the SLCNBB. We worked in teams of two radiographers and one radiologist during the procedure. The radiographers helped the patient to find the most comfortable position on the table. In case of mammographic microcalcifications, specimen radiography was carried out to identify the calcifications in the biopsy specimen.
A pathologist evaluated the histology of specimens. The radiologist collected data regarding the type of mammographic lesion, the type of breast tissue (complete involution of breast tissue, partly completed involution, dense tissue, very dense breast tissue), the biopsy procedure and the histological diagnosis. Written and oral information was given to the patient prior to the SLCNBB. Following their biopsy procedure, the patients were asked to complete a questionnaire (Fig. 1). All 150 patients completed the questionnaire. A fixed interval rating scale was used to score the pain experience and the discomfort.
Statistical analysis
Correlations with P values were computed by means of the Spearman method or general linear modeling where appropriate. The statistical analysis was performed with use of SAS ver. 9.1 software (SAS Corp., Carey, N.C., USA).
Questions were included about the duration of the procedure, discomfort in lying on a prone table, pain experienced in the neck and shoulders, pain experienced in the breast during biopsy, the role of the radiologist. Finally the patient was asked if she would undergo the same procedure if necessary.
Results
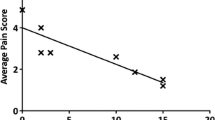
In Table 1, the results are shown of pain in the breast during the procedure. Among the 150 biopsy procedures analysed, 31 patients had complete involution of breast tissue, 83 patients showed partly completed involution of breast tissue, 30 with dense tissue and six with very dense tissue. In Table 2, the distribution of the type of breast tissue is given.
The type of breast tissue is correlated with the pain experienced from biopsy (P = 0.0001). Patients with dense breast tissue experienced more pain than patient with complete involution of breast tissue.
Depth of the biopsy correlates with pain from biopsy (P = 0.0028). The duration of the procedure, the measured length of time, is not correlated with pain experienced from the biopsy.
In Table 3, the results are shown of pain experienced in the neck and shoulder during the procedure. The painscores used in Tables 1 and 3 are the same.
Duration of the procedure ranged from 20 to 75 min with an average time of 37.8 min. Pain in the neck is correlated with the duration of the procedure (P = 0.0116).
There is a correlation between the number of passes and pain in the neck (P = 0.0188) and shoulder (P = 0.0366).
We extended our statistical general linear model to include;multivariate-type of breast tissue, depth of the biopsy and number of passes to ‘predict’ pain scores. Depicted in Table 4 are the beta (slope) parameters and P values. For the categorical variable “type of breast tissue” the beta parameter for the dense or very dense tissue can be interpreted as the average higher pain score in this category compared with women with complete or partly completed involution, corrected for biopsy depth and number of biopsies.
Normal breast tissue was found in three patients, benign tissue in 94 patients, high risk tissue (LCIS, atypical ductal hyperplasia, atypical lobular hyperplasia) in five patients and malignant tissue in 48 patients.
There is no relation between type of breast lesion and pain, underlying pathology and pain and performing operator (male and female) and pain.
In three patients, a haematoma developed just after the procedure. One patient had a vaso-vagal reaction after the procedure. However, no biopsy procedures had to be terminated because of complications.
If necessary all patients stated that they would undergo the same procedure again.
Discussion
Breast cancer is the most common malignancy in women and the leading cause of death for women aged 25–64 years in western countries. Approximately one out of every nine women is diagnosed with breast cancer at some point during her life. The number of breast cancer cases has been increasing worldwide during the past decades. This increase is influenced by a growing and ageing population, a later age at the birth of a first child, earlier menarche, as well as by the introduction of national mammographic screening programs [4].
Diagnostic accuracy in the non-operative diagnosis of breast disease is best achieved by a triple approach which combines the results of clinical examination, imaging with fine-needle aspiration cytology and/or core biopsy. When the results of all three modalities agree, the level of diagnostic accuracy exceeds 99%. Percutaneous needle biopsy should be the standard practice [5]. Percutaneous biopsy is less invasive than surgery and cost effective [6].
It might be expected that type of breast lesion, underlying histology of the lesion or performing operator would influence the degree of discomfort and pain experienced by the patient [3]. However, no associations were found in our study.
Satchithananda et al. [7] also assessed the pain and discomfort experienced during image-guided breast biopsies. The only significant factor in pain scores was the size of the needle used. In our study, we saw a correlation between type of breast tissue and pain. We found out that patients with dense breast tissue complain of more pain from biopsy than patients with more involution of breast tissue. Deep lesions are more painful than superficial ones. These findings are new, and were, to the best of our knowledge, not published before.
Stereotactic large-core needle biopsy seems to affect quality of life to a lesser extent than open breast biopsy. This difference is mainly attributable to a reduction of physical discomfort and pain [8]. In our institution we do not use vacuum-assisted biopsy devices.
The biopsy procedure using vacuum devices is somewhat different than core needles, as samples are collected contiguously, without removing the needle between samples. A larger cavity is produced. Thus, the pain may differ from large-core biopsies, due to decreased length of procedure or larger amount of tissue obtained.
It is important that any discomfort experienced by the patient during a biopsy procedure is minimised. Adequate local anesthesia and comfortable positioning on the table is important. The length of the procedure is proportionate to any pain experienced in the neck.
We use specially trained radiographers and radiologists for the SLCNBB. Written and oral information is given to the patient prior to the SLCNBB. Van Goethem et al. [9] showed that the information and communication during mammography are important factors in minimising pain and discomfort. An experienced team can shorten procedure times. Short procedure times mean less patient discomfort, as shown by Mainieiro et al. [10].
Conclusion
Stereotactic large-core needle breast biopsy is a safe and reliable procedure, which is not experienced as painful in 60% of our patients. It is important that any discomfort experienced by the patient during a biopsy procedure is minimised. Adequate local anesthesia and comfortable positioning on the table is important. There is a correlation between duration of the procedure and pain in the neck. Patients with dense glandular breast tissue with a deep lesion experience more pain during stereotactic large-core needle breast biopsy.
References
Huber S, Wagner M, Medl M, Czembirek H (2003) Minimally invasive vacuum-assisted biopsy with 11-gauge needles—patient acceptance and effect on follow-up imaging findings. Radiology 226(3):783–790
Oyama T, Koibuchi Y, McKee G (2004) Core needle biopsy (CNB) as a diagnostic method for breast lesions: comparison with fine needle aspiration cytology (FNA). Breast Cancer 11(4):339–342
Denton ERE, Ryan S, Beaconfield T, Mitchell MJ (1999) Image-guided breast biopsy: analysis of pain and discomfort related to technique. Breast 8(5):257–260
Fletcher SW, Elmore JG (2003) Clinical practice. Mammographic screening for breast cancer. N Engl J Med 348(17):1672–1680
Wallis M, Tarvidon A, Helbich Th, Schreer I (2007) Guidelines from the European Society of breast imaging for diagnostic interventional breast procedures. Eur Radiol 17(2):581–588
Liberman L (2000) Centennial dissertation. Percutaneous image-guided core breast biopsy: state of the art at the millennium. AJR Am J Roentgenol 174(5):1191–1199
Satchithananda K, Fernando RA, Ralleigh G, Evans DR, Wasan RK, Bose S, Donaldson N, Michell MJ (2005) An audit of pain/discomfort experienced during image-guided breast biopsy procedures. Breast 11(6):398–402
Verkooijen HM, Buskens F, Peeters PH, Borel Rinkes IH, de Koning HJ, van Vroonhoven TJ; COBRA Study Group (2002) Diagnosing non-palpable breast disease: short-term impact on quality of life of large-core needle biopsy versus open breast biopsy. Surg Oncol 10(4):177–181
van Goethem M, Mortelmans D, Bruyninckx E, Verslegers I, Biltjes I, van Hove E, de Schepper A (2003) Influence of the radiographer on the pain felt during mammography. Eur Radiol 13(10)2384–2389
Mainiero MB, Gareen IF, Bird CE, Smith W, Cobb C, Schepps B (2002) Preferential use of sonographically guided biopsy to minimize patient discomfort and procedure time in a percutaneous image-guided breast biopsy program. J Ultrasound Med 21(11):1221–1226
Acknowledgements
We are grateful for all the help and valuable advice provided by M. van der Spek-Heijning, MA.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 2.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made.
The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
To view a copy of this licence, visit https://creativecommons.org/licenses/by-nc/2.0/.
About this article
Cite this article
Hemmer, J.M., Kelder, J.C. & van Heesewijk, H.P.M. Stereotactic large-core needle breast biopsy: analysis of pain and discomfort related to the biopsy procedure. Eur Radiol 18, 351–354 (2008). https://doi.org/10.1007/s00330-007-0762-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-007-0762-3