Abstract
Aims/hypothesis
Increased expression and decreased degradation of extracellular matrix (ECM) proteins are key features of chronic diabetic complications. Fibronectin, a predominant ECM protein, has been shown to be overexpressed in all target organs of diabetic complications and in endothelial cells cultured in high levels of glucose. The present study was designed to elucidate the role of protein kinase B (Akt/PKB) in glucose-induced fibronectin mRNA expression and protein production in vascular endothelial cells.
Methods
Human umbilical vein endothelial cells were cultured in the presence of high glucose to study Akt/PKB activation. The upstream and downstream mediators in the Akt/PKB pathway were also investigated using dominant negative transfections and specific inhibitors of signalling pathways. Cells were subjected to real time RT-PCR, western blotting, and confocal microscopy to assess Akt1/PKBα activation and fibronectin mRNA expression and protein production. To detect transcription factor activation, electrophoretic mobility shift assay was carried out.
Results
Our data demonstrate that fibronectin mRNA expression and protein production that are induced by high glucose are mediated via activation of Akt/PKB, which is modulated by mitogen-activated protein kinase, phosphatidylinositol 3-kinase, and protein kinase C. Glucose-induced fibronectin mRNA expression and protein production are also mediated by Akt1/PKBα-dependent activation of the transcription factors nuclear factor-κB and activating protein-1.
Conclusions/interpretation
Our study provides insight into the mechanical basis of glucose-induced increases in fibronectin mRNA expression and protein production. High levels of glucose may increase fibronectin mRNA expression and protein production by activating Akt/PKB.
Similar content being viewed by others
Introduction
Increased extracellular matrix (ECM) protein production and impaired degradation are important features of chronic diabetic complications [1, 2]. This imbalance is instrumental in producing the structural hallmark of diabetic complications, basement membrane thickening. One predominant ECM protein that is upregulated in diabetic angiopathy is fibronectin [3, 4]. Fibronectin is a highly specialised glycoprotein of 250 kDa. These ECM proteins interact with other matrix proteins and modulate cellular processes by interacting with cell surface receptors [5–7]. We and others have previously demonstrated the upregulation of fibronectin mRNA in vascular endothelial cells exposed to high levels of glucose and in the target organs of diabetic complications, i.e. retina, kidney and heart [3, 4]. We have further demonstrated that these alterations may, in part, be dependent on the hyperglycaemia-induced increase in the production of vasoactive factors such as endothelins (ETs) and subsequent activation of nuclear factor-κB (NF-κB) and activating protein-1 (AP-1) [8, 9].
Sustained hyperglycaemia in diabetes and high levels of glucose in cultured endothelial cells may modify various growth factors that lead to biochemical anomalies. Such molecular changes may arbitrate glucose-induced signals for fibronectin mRNA expression. We have previously demonstrated that mitogen-activated protein kinase (MAPK) and protein kinase C (PKC) may cause fibronectin mRNA and protein upregulation [10]. It is increasingly being realised that such protein kinase pathways may also interact and cross-talk with cellular process regulation [11, 12]. One such key kinase pathway involved in glucose-induced fibronectin upregulation may be phosphatidylinositol 3-kinase (PI 3-kinase)-dependent protein kinase B (Akt/PKB). Akt is a widely expressed serine/threonine kinase [13] that has been identified as an important component of several signalling pathways [14]. Upon stimulation with growth factors, PI 3-kinase mediates the phosphorylation of Akt, which interacts with intracellular signalling molecules to promote cell survival. Such survival signals are regulated by the activity of proapoptotic proteins, transcription factors, and by cell–cell and cell–matrix interactions [15–17]. Some reports indicate that apparently separate and important signalling pathways, such as MAPK and the transcription factors NF-κB and AP-1, may be modulated by Akt [18–22]. Hence, it is plausible that Akt-dependent NF-κB and AP-1 activation may lead to the upregulation of fibronectin mRNA expression in diabetic patients.
This study was conducted to elucidate the mechanisms of glucose-induced increases in mRNA expression and protein production of fibronectin in endothelial cells. Specifically, we wanted to address whether such phenomena are mediated via Akt1/PKBα phosphorylation and Akt1/PKBα-dependent NF-κB/AP-1 activation. To study the role of Akt1/PKBα in fibronectin production, we used human vascular endothelial cells. Human endothelial cells cultured in the presence of high levels of glucose increased mRNA expression and protein production of many basement membrane proteins, including fibronectin, thus mimicking the effects of diabetes [9, 23, 24].
Materials and methods
Reagents
Unless otherwise stated, all reagents were obtained from Sigma Chemicals (Sigma, Oakville, ON, Canada).
Cell culture and transfections
Human umbilical vein endothelial cells (Clonetics, Walkersville, MD, USA) were cultured as previously described [9]. Briefly, the HUVECs were cultured to 80% confluence in EGM growth medium (Clonetics) before the treatments were carried out. l-glucose was used as a control.
Dominant negative Akt (Akt-K179M) constructs were a gift from Dr Bruce McManus and Dr Esfandiarei (Department of Pathology and Laboratory Medicine, University of British Columbia, Canada). Wild-type Akt1/PKBα (Akt-1-WT) was obtained from Upstate Biotech Company (Upstate USA, Chicago, IL, USA). Sub-confluent cells were transfected with 5 μg of DNA per flask using lipofectin (Invitrogen Canada, Burlington, ONo, Canada) under serum-free conditions for 6 h, after which the cells were replenished with culture medium for 24 h. The transfection efficiency was 25%, as determined by pCMVB-galactosidase. Cells were incubated with either 5 mmol/l d-glucose (control) or 25 mmol/l d-glucose (high glucose; HG). To elucidate the signalling pathways, cells in HG were pretreated with the following: Akt inhibitor ML-9 (100 μmol/l; Cedarlane Laboratories, Hornby, ON, Canada); the dual ET receptor antagonist bosentan (10 μmol/l; courtesy of M. Clozel, Actelion, Allschwill, Switzerland); the PKC inhibitor chelerythrine (1 μmol/l, Sigma-Aldrich, Oakville, ON, Canada); the MAPK inhibitor PD98059 (50 μmol/l; Fisher Scientific, Nepean, ON, Canada); and the PI 3-kinase inhibitors LY294002 (25 μmol/l; Sigma-Aldrich) and wortmannin (100 μmol/l; Sigma). All pre-treatments were carried out for 1 h before exposure to HG.
Following treatments, RNA was extracted for fibronectin gene expression analysis by real time RT-PCR. The protein extracts were used for western blot analysis and Akt kinase assay. In addition, nuclear proteins were isolated for analysis of NF-κB and AP-1 transcription factor activation. Unless otherwise indicated, all experiments were carried out after 24 h of incubation. Three different batches of cells, each in duplicate, were investigated.
Cell viability
We used crystal violet assay to measure cell viability and exclude potential cytotoxic effects of the inhibitors. HUVECs were seeded in 96-well microtitre plates. Confluent cells were treated with various concentrations of reagents as stated above and examined at different time points. Following treatment, the cells were washed with PBS buffer, fixed with methanol for 5 min, and then stained for 10 min with a 0.1% crystal violet solution. Following three washes, the dye was eluted with 0.1 mol/l trisodium citrate in 50% ethanol for 10 min. The optical density at 630 nm was monitored on a microtitre plate reader (MR 7000; Dynatech Laboratories, Chantilly, VA, USA).
Real-time RT-PCR
RNA was extracted and subjected to cDNA synthesis as described [9]. Real-time quantitative RT-PCR for fibronectin gene expression was carried out in a LightCycler (Roche Diagnostics Canada, Laval, QC, Canada) using SYBR Green I. PCR was performed essentially as described previously [9]. The reaction mixture consisted of 10 μl of ReadyMix SYBR (Sigma-Aldrich), 1.6 μl of 25 mmol/l MgCl2, 1 μl each of forward and reverse 10 μmol/l primers (Table 1), 5.4 μl H2O, and 1 μl cDNA template. The mRNA levels were quantified using the standard curve method. Standard curves were constructed by using a serially diluted standard template. The data were normalised to 18S rRNA [25] to account for differences in reverse transcription efficiencies.
Protein analysis
Total proteins from HUVECs were isolated using complete RIPA buffer (NaCl 0.877 g, deoxycholate 1 g, 1 mol/l Tris–HCl pH 7.5 5 ml, and 10% sodium dodecyl sulphate 1 ml; volume adjusted to 100 ml using double-distilled H2O) and protease inhibitors. Total proteins were then quantified using the Bio-Rad protein assay procedure (Pierce Endogen, Rockford, IL, USA). Akt1/PKBα protein activation was assessed using phospho-Akt (Ser473) antibody (1:1000; New England BioLabs, Pickering, ON, Canada). The fibronectin protein was assessed using anti-fibronectin polyclonal antibody (1:2000; DakoCytomation California, Carpinteria, CA, USA). Western blots were detected with the ECL-Plus kit (Amersham Pharmacia Biotech, Piscataway, NJ, USA).
Akt kinase assay
The cells were subjected to Akt kinase assay in accordance with the manufacturer’s recommendations (New England BioLabs). Ice-cold cell lysis buffer with 1 mmol/l phenylmethylsulphonyl fluoride was added to the samples. The samples were sonicated and centrifuged at 1,500 g for 10 min. The pellets were suspended in 40 μl 1× kinase buffer supplemented with 200 μmol/l ATP and substrates. The reaction was terminated with 20 μl of 3× SDS sample buffer. The samples were then centrifuged for 30 s, heated to 95–100°C for 2–5 min, and loaded on SDS-PAGE gel (12–15%) for sample analysis by Western blotting.
Immunofluorescent microscopy
Endothelial cells were cultured in 12-well plates (Fisher Scientific) with coverslips. Transfected cells were treated with glucose and inhibitors for 24 h as described earlier. Following treatment, cells were fixed in anhydrous ethanol and probed with polyclonal rabbit anti-human fibronectin antibody (1:1000; Dako Diagnostics Canada, Mississauga, ON, Canada). FITC-labelled goat anti-rabbit secondary antibody (Vector Laboratories) was used for detection, with a confocal microscope equipped with UV and FITC/TRITC filters (Zeiss LSM 410; Carl Zeiss Canada, Toronto, ON, Canada).
Electrophoretic mobility shift assay
Nuclear extracts were prepared essentially as described [9]. Rapid detection of octamer binding proteins with ‘mini-extracts’ was prepared from a small number of cells. Briefly, the cells were washed, resuspended in PBS, and centrifuged (7,000 g for 15 s). The pellet was resuspended in 0.4 ml of cold buffer A (10 mmol/l HEPES, pH 7.9, 10 mmol/l KCl, 0.1 mmol/l EDTA, 0.1 mmol/l EGTA, 1 mmol/l 1,4-dithiothreitol, and 0.5 mmol/l phenylmethylsulphonyl fluoride). The cells were allowed to swell on ice for 15 min. Next, 25 μl of 10% IGEPAL CA-630 was added. The homogenate was centrifuged (10,000 g for 30 s). The nuclear pellet was resuspended in 50 μl of ice-cold buffer C (20 mmol/l HEPES, pH 7.9, 0.4 mol/l NaCl, 1 mmol/l EDTA, 1 mmol/l EGTA, 1 mmol/l 1,4-dithiothreitol, and 1 mmol/l phenylmethylsulphonyl fluoride) at 4°C for 15 min on a shaking platform. The nuclear extracts were centrifuged at 4°C (15,000 g for 5 min), and the supernatant was frozen at −70°C. The protein concentrations were measured using the BCA protein assay, with bovine serum albumin as a standard (Pierce). Electrophoretic mobility shift assay (EMSA) was performed as described previously [9]. Briefly, NF-κB consensus oligonucleotide DNA probes (Promega, Madison, WI, USA) (Table 2) were prepared by end-labelling with [γ-32P]ATP (Amersham, Baie d’Urfe, QC, Canada) using T4 polynucleotide kinase. The probes were purified by ethanol precipitation and resuspended in 10 mmol/l Tris and 1 mmol/l EDTA (pH 7.6). Next, 5 μl of nuclear proteins were incubated with 100,000 cpm of 32P-labelled consensus oligonucleotides for 30 min at room temperature. The incubation was carried out in a buffer containing 10 mmol/l Tris (pH 7.5), 50 mmol/l NaCl, 1 mmol/l MgCl2, 5% glycerol, 0.05% IGEPAL CA-630, 0.5 mmol/l EDTA, 0.5 mmol/l 1,4-dithiothreitol, and 0.5 μg of poly (dI-dC). Protein–DNA complexes were resolved on a standard 6% (NF-κB) and 4% (AP-1) non-denaturing polyacrylamide gel in 0.5× Tris–boric acid–EDTA running buffer. After 30 min of electrophoresis at 350 V, gels were dried under heated vacuum on to Whatman paper and subjected to autoradiography from overnight to three days. The specificity was established by supershift assay using NF-κB-p50 and AP-1/c-Jun antibodies, and by incubation with cold probe. The blots were quantified by densitometry [9].
Statistical analysis
The data are expressed as means±SEM and were analysed by ANOVA followed by t-test with Bonferroni’s correction as appropriate. Differences were considered significant at values of p<0.05.
Results
Glucose induces fibronectin mRNA upregulation in endothelial cells
Exposure of endothelial cells to high (25 mmol/l) glucose causes a duration-dependent increase in the mRNA expression of fibronectin, reaching a maximum level after 24 h of exposure (Fig. 1). Cells exposed to 25 mmol/l glucose showed an increase in immunocytochemically detectable fibronectin protein production (Fig. 2). No alteration of fibronectin expression was seen in cells exposed to l-glucose.
Quantitative analysis of fibronectin (FN) mRNA expression in the endothelial cells exposed to glucose as determined by real-time PCR. a The melting curve analysis. Each line represents PCR amplification of individual cDNA samples. b Upregulation of fibronectin mRNA expression by 25 mmol/l glucose, which was prevented by the Akt inhibitor ML-9. Open bar, low glucose (5 mmol/l glucose); black bar, high glucose (25 mmol/l glucose); grey bar, high glucose + ML-9 (100 μmol/l in HG). *p<0.05 vs low glucose. c Duration-dependent increase in glucose-induced fibronectin expression with wild-type Akt1/PKBα transfection (Akt-1-WT, open bar) and normalisation with dominant negative Akt transfection (Akt/PKB-K179M, black bar), or treatment with ML-9 (grey bar). *p<0.05 vs Akt1/PKBα -WT at 0 h; n=4 per treatment
a–h Immunofluorescent analysis of fibronectin protein production. Endothelial cells (a) 5 mmol/l glucose, (b) 25 mmol/l glucose, exposed to (c) with Akt-1-WT transfection in 5 mmol/l glucose, (d) with Akt-1-WT transfection in 25 mmol/l glucose, (e) with Akt-1-WT transfection in 25 mmol/l glucose + ML-9, (f) with Akt-1-WT transfection in 25 mmol/l glucose + wortmannin, (g) with Akt-K179M transfection in 5 mmol/l glucose, and (h) with Akt-K179M transfection in 25 mmol/l glucose. Note the reduced immunoreactivity in panels e–h. i A representative fibronectin western blot, and j semiquantification of the bonds by densitometry. *p<0.05 vs non-transfected HUVECs on 5 mmol/l glucose (open bars). Black bars, high glucose (25 mmol/l). β-actin was used as a loading control
Glucose induces fibronectin mRNA up-regulation in endothelial cells via Akt1/PKBα activation
We evaluated the effect of a chemical inhibitor of Akt activation, ML-9. ML-9 pretreatment completely abolished glucose-induced fibronectin up-regulation (Fig. 1). Furthermore, cells transfected with Akt-1-WT demonstrated fibronectin mRNA up-regulation following exposure to 25 mmol/l of glucose. Such up-regulation was blocked by ML-9 pretreatment. A significant reduction (approximately 80%) in fibronectin mRNA expression was observed in the cells with dominant negative Akt transfection (Akt-K179M; Fig. 1). Moreover, the production of fibronectin protein as detected immunocytochemically or by western blots corresponded to the mRNA data (Fig. 2).
Western blot analysis, using Akt and phospho-Akt antibodies, showed a significant prevention of Akt1/PKBα activation following dominant negative transfection compared with cells with wild-type transfection (Fig. 3). Akt kinase assay also revealed a significant activation of glycogen synthase kinase-3, a downstream protein in the Akt pathway, in cells transfected with Akt-1-WT, compared with those transfected with Akt-dominant negative constructs (Fig. 3). However, a slight, transient increase in glycogen synthase kinase (GSK)-3 activity was seen in 24 h dominant-negative-transfected cells exposed to glucose after, which may represent basal activity. No significant increase in cell death was observed after 24 h of transfection (data not shown). A similar prevention of Akt1/PKBα activation was demonstrated when HUVECs exposed to 25 mmol/l of glucose were treated with the chemical Akt inhibitor ML-9 (Fig. 4).
a Representative western blot showing prevention of Akt1/PKBα phosphorylation by dominant negative transfection. b Quantitative analysis of Akt1/PKBα phosphorylation. c Western blot of GSK activity. d Quantitative analysis of the Akt kinase assay. Control was HUVECs without transfections (open bars). Black bars, AKT-K179M; grey bars, Akt-WT. *p<0.05 vs control and 0 h of respective treatment
Transcription factor involvement in Akt1/PKBα-mediated signalling of fibronectin mRNA expression
EMSA results revealed glucose-induced activation of NF-κB and AP-1 in Akt1-WT endothelial cells. Transfection of HUVECs with Akt-K179M prevented glucose-mediated NF-κB and AP-1 activation (Fig. 5).
a EMSA showing glucose-induced activation of NF-κB. b Quantitative analysis of NF-κB binding activity. c EMSA of glucose-induced activation of AP-1. d Quantitative analysis of AP-1 binding activity. Low glucose (LG)=5 mmol/l glucose; high glucose (HG)=25 mmol/l glucose. Black bars, Akt-K179M; grey bars, Akt-WT. The specificity of the EMSA was confirmed by supershift assay and incubation with cold probe (data not shown). n=4 per treatment. *p>0.05 vs Akt-K179M HG; †p<0.05
Mechanisms of glucose-induced Akt activation
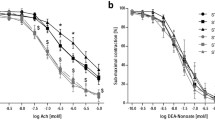
In endothelial cells exposed to high levels of glucose, the inhibition of ET signalling by the dual ET receptor antagonist bosentan prevented Akt activation (Fig. 6). The inhibitors that prevented glucose-induced Akt1/PKBα activation also prevented the downstream effects such as fibronectin mRNA expression (data not shown).
a ET-1-induced Akt activation levels as determined by a representative western blot. Lane 1, control (HUVECs without any treatment); lanes 2 and 7, low glucose (LG), 5 mmol/l glucose; lanes 3 and 8, high glucose (HG), 25 mmol/l glucose; lanes 4 and 9, ET-1 (5 nmol/l ET-1 peptide alone); lanes 5 and 10, HG + Bos (10 μmol/l bosentan); and lanes 6 and 11, HG + ML-9 (100 μmol/l ML-9). b Quantitative analysis of the blot. Black bars, Akt-K179M; grey bars, Akt-WT. *p<0.05 vs control and respective LG; n=4 per treatment
Our results also indicate that glucose-induced Akt1/PKBα activation was prevented, in part, by the MAPK inhibitor PD98059, the PKC inhibitor chelerythrine, and the PI 3-kinase inhibitors LY294002 and wortmannin (Fig. 4). These compounds also prevented glucose-induced fibronectin mRNA upregulation (data not shown).
Cell viability
The concentrations used in the viability assay included the working concentration of the inhibitors. No significant changes in cell viability were observed following treatment with specific signalling pathway inhibitors (data not shown).
Discussion
The results of this study provide evidence of a novel mechanical pathway by which high levels of glucose may cause increased fibronectin mRNA expression and protein production via activation of Akt1/PKBα signalling in endothelial cells. We have also shown that high glucose induces ET-1-mediated Akt1/PKBα activation, in part, by the PKC and MAPK pathways. Such activation of Akt1/PKBα mediates fibronectin expression by the transcription factors NF-κB and AP-1.
The serine/threonine kinase Akt may influence several signalling pathways and may act as an inducer of multiple cellular functions including gene expression [26]. Akt may also influence diverse cellular processes such as glucose metabolism, apoptosis, cell proliferation, and angiogenesis [27]. In the present study, we have established another novel cellular pathophysiological role of Akt, namely the glucose-induced increase in fibronectin production by endothelial cells. Increased ECM protein production is a key feature of chronic diabetic complications and is structurally manifested as thickening of the capillary basement membrane in the target organs of diabetic complications [28]. Increased production of ECM proteins, such as fibronectin, may be an important factor leading to the development of long-term changes such as angiogenesis in diabetic retinopathy [3, 29]. Several biochemical anomalies induced by high glucose may activate Akt. Results from this study suggest that PI-3-kinase-mediated Akt activation is one of the key mechanisms for the induction of such anomalies [30]. However, other mechanisms, such as activation of 3-phosphoinositide-dependent-kinase or PI 3-kinase-independent mechanisms, which have been demonstrated in other systems, may be of potential importance in the current scenario [30, 31]. Our studies also demonstrate that MAPK and PKC may, in part, activate Akt1/PKBα. Such activation may occur via G-protein-coupled receptor signalling such as ETs, as well as other factors, e.g. oxidative stress [29]. Interestingly, hyperglycaemia-induced PKC activation may activate ET-1 [32], and ET-1, in turn, may activate PKC.
We have previously demonstrated that ET-1-induced fibronectin production in response to high levels of glucose is also mediated by the transcription factors NF-κB and AP-1 [8, 9]. We have also demonstrated that ET-induced fibronectin mRNA production may also be mediated via MAPK signalling [10]. Moreover, the current study and other investigations in the literature indicate that MAPK may influence PKB activation [19, 33]. Akt activation is known to influence the activation of the transcription factor NF-κB in other systems [34]. Similarly, the transcription factor AP-1 may also be regulated by Akt1/PKBα [35]. The fibronectin gene promoter has both NF-κB and AP-1 binding sites and may be positively regulated by both transcription factors [36]. High levels of glucose may activate NF-κB via the NF-κB-inducing kinase or a mechanism yet to be identified [37, 38]. In addition, Akt1/PKBα may activate AP-1 by phosphorylating downstream GSK-3β [20, 38].
Taken together, our study and previous findings suggest that high levels of glucose may activate Akt through parallel modification of ETs and activation of kinase pathways such as PKC and MAPK. The activation of Akt subsequently sequesters the positive transcriptional regulation of NF-κB and AP-1, leading to increased fibronectin expression. However, the notion that hyperglycaemia may lead via similar biochemical pathways to increased fibronectin expression in target organs of patients with late complications of diabetes requires further investigation. Such a notion is supported by findings indicating that ET-1 may cause PI 3-kinase-mediated Akt1/PKBα activation in other systems [39]. It is also possible that other pathways of Akt1/PKBα activation exist in patients with diabetes. It is also unclear how other well established glucose-induced mechanisms such as augmentation of the polyol pathway, non-enzymatic glycation and mitochondrial superoxide production interact with Akt/PKBα activation. It remains to be investigated whether other ECM proteins follow similar pathways. The identification of such novel mechanical pathways is important, as they may offer potential drug targets.
Abbreviations
- Akt/PKB:
-
protein kinase B
- Akt-1-WT:
-
wild-type Akt1/PKBα
- Akt-K179M:
-
dominant negative Akt
- AP-1:
-
activating protein-1
- ECM:
-
extracellular matrix
- EMSA:
-
electrophoretic mobility shift assay
- ET:
-
endothelin
- GSK:
-
glycogen synthase kinase
- HG:
-
25 mmol/l d-glucose, high glucose
- MAPK:
-
mitogen-activated protein kinase
- NF-κB:
-
nuclear factor-κB
- PI 3-kinase:
-
phosphatidylinositol 3-kinase
- PKC:
-
protein kinase C
References
King, GL, Brownlee M (1996) The cellular and molecular mechanisms of diabetic complications. Endocrinol Metab Clin North Am 25:255–270
Khan ZA, Chakrabatri S (2003) Endothelins in chronic diabetic complications. Can J Physiol Pharmacol 8:622–634
Khan ZA, Cukiernik M, Gonder J, Chakrabarti S (2004) Oncofetal fibronectin in diabetic retinopathy. Invest Ophthalmol Vis Sci 45:287–295
Roy S, Cagliero E, Lorenzi M (1996) Fibronectin overexpression in retinal microvessels of patients with diabetes. Invest Ophthalmol Vis Sci 37:258–266
Yamada KM (1983) Cell surface interactions with extracellular materials. Annu Rev Biochem 52:761–799
Isono M, Cruz MC, Chen S, Hong SW, Ziyadeh FN (2000) Extracellular signal-regulated kinase mediates stimulation of TGF-beta1 and matrix by high glucose in mesangial cells. J Am Soc Nephrol 11:2222–2230
Bowlus CL, McQuillan JJ, Dean DC (1991) Characterization of three different elements in the 5′-flanking region of the fibronectin gene which mediate a transcriptional response to cAMP. J Biol Chem 266:1122–1127
Chen S, Khan ZA, Cukiernik M, Chakrabarti S (2003) Differential activation of NF-κB and AP-1 in increased fibronectin synthesis in target organs of diabetic complications. Am J Physiol Endocrinol Metab 284:E1089–E1097
Chen S, Mukherjee S, Chakraborty C, Chakrabarti S (2003) High glucose-induced, endothelin-dependent fibronectin synthesis is mediated via NF-κB and AP-1. Am J Physiol Cell Physiol 284:C263–C272
Xin X, Khan ZA, Chen S, Chakrabarti S (2004) Extracellular signal-regulated kinase (ERK) in glucose-induced and endothelin-mediated fibronectin synthesis. Lab Invest 84:1451–1459
Haneda M, Kikkawa R, Sugimoto T et al. (1995) Abnormalities in protein kinase C and MAP kinase cascade in mesangial cells cultured under high glucose conditions. J Diabetes Complicat 9:246–248
Eccles SA (2004) Parallels in invasion and angiogenesis provide pivotal points for therapeutic intervention. Int J Dev Biol 48:583–598
Scheid MP, Woodgett JR (2001) PKB/AKT functional insights from genetic models. Nat Rev Mol Cell Biol 2:760–768
Pap M, Cooper GM (1998) Role of glycogen synthase kinase-3 in the phosphatidylinositol 3-kinase/Akt cell survival pathway. J Biol Chem 273:19929–19932
Wang XQ, Sun P, Paller AS (2001) Inhibition of integrin-linked kinase/protein kinase B/Akt signaling: mechanism for ganglioside-induced apoptosis. J Biol Chem 276:44504–44511
Khwaja A (1999) Akt is more than just a Bad kinase. Nature 401:33–34
Ozes ON, Mayo LD, Gustin JA, Pfeffer SR, Pfeffer LM, Donner DB (1999) NF-kappa B activation by tumour necrosis factor requires the Akt serine–threonine kinase. Nature 401:82–85
Tomlinson DR (1999) Mitogen-activated protein kinases as glucose transducers for diabetic complications. Diabetologia 42:1271–1281
Gold MR, Ingham RJ, McLeod SJ et al. (2000) Targets of B-cell antigen receptor signaling: the phosphatidylinositol 3-kinase/Akt/glycogen synthase kinase-3 signaling pathway and the Rap1 GTPase. Immunol Rev 176:47–68
Troussard AA, Tan C, Yoganathan TN, Dedhar S (1999) Cell–extracellular matrix interactions stimulate the AP-1 transcription factor in an integrin-linked kinase- and glycogen synthase kinase 3-dependent manner. Mol Cell Biol 19:7420–7427
Doble BW, Woodgett JR (2003) GSK-3: tricks of the trade for a multi-tasking kinase. J Cell Sci 116:1175–1186
Perez OD, Nolan GP (2002) Simultaneous measurement of multiple active kinase states using polychromatic flow cytometry. Nat Biotechnol 20:155–162
Cagliero E, Roth T, Roy S, Maiello M, Lorenzi M (1991) Expression of genes related to the extracellular matrix in human endothelial cells. Differential modulation by elevated glucose concentrations, phorbol esters, and cAMP. J Biol Chem 266:14244–14250
Roy S, Roth T (1997) Proliferative effect of high glucose is modulated by antisense oligonucleotides against fibronectin in rat endothelial cells. Diabetologia 40:1011–1017
Schmittgen TD, Zakrajsek BA (2000) Effect of experimental treatment on housekeeping gene expression: validation by real-time, quantitative RT-PCR. J Biochem Biophys Methods 46:69–81
Kandel ES, Hay N (1999) The regulation and activities of the multifunctional serine/threonine kinase Akt/PKB. Exp Cell Res 253:210–229
Brazil DP, Hemmings BA (2001) Ten years of protein kinase B signalling: a hard Akt to follow. Trends Biochem Sci 26:657–664
Brownlee M (2001) Biochemistry and molecular cell biology of diabetic complications. Nature 414:813–820
Evans T, Deng DX, Chakrabarti S (2000) Endothelin receptor blockade prevents augmented extracellular matrix protein component mRNA expression and capillary basement membrane thickening in the retina of diabetic and galactose fed rats. Diabetes 49:662–666
Downward J (1998) Mechanisms and consequences of activation of protein kinase B/Akt. Curr Opin Cell Biol 10:262–267
Craddock BL, Orchiston EA, Hinton HJ, Welham MJ (1999) Dissociation of apoptosis from proliferation, protein kinase B activation, and BAD phosphorylation in interleukin-3-mediated phosphoinositide 3-kinase signaling. J Biol Chem 274:10633–10640
Ishii H, Koya D, King GL (1998) Protein kinase C activation and its role in the development of vascular complications in diabetes mellitus. J Mol Med 76:21–31
Bozinovski S, Jones JE, Vlahos R, Hamilton JA, Anderson GP (2002) Granulocyte/macrophage-colony-stimulating factor (GM-CSF) regulates lung innate immunity to lipopolysaccharide through Akt/ERK activation of NFkappa B and AP-1 in vivo. J Biol Chem 277:42808–42814
Meng F, Liu L, Chin PC, D’Mello SR (2002) Akt is a downstream target of NF-κB. J Biol Chem 277:29674–29680
Chen Li H, Tang MS, Shi X (2004) PI-3K and Akt are mediators of AP-1 induction by 5-MCDE in mouse epidermal Cl41 cells. J Cell Biol 165:77–86
Kane LP, Mollenauer MN, Xu Z, Turck CW, Weiss A (2002) Akt-dependent phosphorylation specifically regulates Cot induction of NF-kappa B-dependent transcription. Mol Cell Biol 22:5962–5974
Chen F, Castranova V, Shi X (2001) New insights into the role of nuclear factor-kappaB in cell growth regulation. Am J Pathol 159:387–397
Kane LP, Shapiro VS, Stokoe D, Weiss A (1999) Induction of NF-kappaB by the Akt/PKB kinase. Curr Biol 11:601–604
Ishibashi KI, Imamura T, Sharma PM, Huang J, Ugi S, Olefsky JM (2001) Chronic endothelin-1 treatment leads to heterologous desensitization of insulin signaling in 3T3-L1 adipocytes. J Clin Invest 107:1193–1202
Acknowledgements
The study was supported by grants from the Canadian Diabetes Association, in honour of the late Glenn W. Liebrock, and from the Canadian Institutes of Health Research, and the Lawson Health Research Institute.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Xin, X., Khan, Z.A., Chen, S. et al. Glucose-induced Akt1 activation mediates fibronectin synthesis in endothelial cells. Diabetologia 48, 2428–2436 (2005). https://doi.org/10.1007/s00125-005-1939-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-005-1939-4