Abstract
Background
The best available treatment of patients with one to three brain metastases is still unclear. This study compared the results of stereotactic radiosurgery (SRS) alone and whole brain radiotherapy (WBRT) plus SRS (WBRT + SRS).
Patients and Methods
Survival (OS), intracerebral control (IC), and local control of treated metastases (LC) were retrospectively analyzed in 144 patients receiving SRS alone (n = 93) or WBRT + SRS (n = 51). Eight additional potential prognostic factors were evaluated: age, gender, Eastern Cooperative Oncology Group performance score (ECOG-PS), tumor type, number of brain metastases, extracerebral metastases, recursive partitioning analysis (RPA) class, and interval from tumor diagnosis to irradiation. Subgroup analyses were performed for RPA class I and II patients.
Results
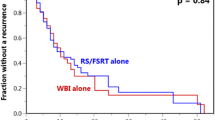
1-year-OS was 53% after SRS and 56% after WBRT + SRS (p = 0.24). 1-year-IC rates were 51% and 66% (p = 0.015), respectively. 1-year-LC rates were 66% and 87% (p = 0.003), respectively. On multivariate analyses, OS was associated with age (p = 0.004), ECOG-PS (p = 0.005), extracerebral metastases (p < 0.001), RPA class (p < 0.001), and interval from tumor diagnosis to irradiation (p < 0.001). IC was associated with interval from tumor diagnosis to irradiation (p = 0.004) and almost with treatment (p = 0.09), and LC with treatment (p = 0.026) and almost with interval (p = 0.08). The results of the subgroup analyses were similar to those of the entire cohort. The increase in IC was stronger in RPA class I patients.
Conclusion
WBRT + SRS resulted in better IC and LC but not better OS than SRS alone. Because also IC and LC are important end-points, additional WBRT appears justified in patients with one to three brain metastases, in particular in RPA class I patients.
Zusammenfassung
Hintergrund
Die bestmögliche Behandlung von Patienten mit 1 bis 3 Hirnmetastasen ist unklar. Diese Studie vergleicht die Ergebnisse der alleinigen Radiochirurgie (SRS) mit den Ergebnissen nach Ganzhirnbestrahlung plus stereotaktischem Boost (WBRT + SRS).
Patienten und Methodik
Gesamtüberleben, intrazerebrale Kontrolle (IC) und lokale Kontrolle der behandelten Metastasen (LC) wurden retrospektiv bei 144 Patienten (93 SRS, 51 WBRT + SRS) ausgewertet (Tabelle 1). Acht weitere mögliche Prognosefaktoren wurden untersucht: Alter, Geschlecht, Allgemeinzustand, Primärtumor, Zahl der Hirnmetastasen, extrazerebrale Metastasierung, RPA-(Recursive-Partitioning-Analysis-)Klasse und Intervall von Erstdiagnose der Tumorerkrankung bis Strahlentherapie. Für die RPA-Klassen I und II wurden Subgruppenanalysen durchgeführt.
Ergebnisse
Das Gesamtüberleben nach 1 Jahr betrug 53% nach SRS und 56% nach WBRT + SRS (p = 0,24) (Abbildung 1, Tabelle 2). Die Raten für die 1-Jahres-IC waren 51% und 66% (p = 0,015), die Raten für die 1-Jahres-LC 66% und 87% (p = 0,003) (Abbildungen 1 und 2, Tabellen 3 und 4). In der Multivarianzanalyse war das Gesamtüberleben mit dem Alter (p = 0,004), dem Allgemeinzustand (p = 0,005), extrazerebraler Metastasierung (p < 0,001), RPA-Klasse (p < 0,001) und dem Intervall von Erstdiagnose bis Strahlentherapie (p < 0,001) assoziiert. Die IC war mit dem Intervall (p = 0,004) und annähernd mit dem Behandlungsregime (p = 0,09), die LC mit dem Behandlungsregime (p = 0,026) und annähernd mit dem Intervall assoziiert (p = 0,08). Die Ergebnisse der Subgruppenanalysen waren denen der Gesamtstudie vergleichbar, wobei die Verbesserung der IC in der RPA-Klasse I ausgeprägter war (Tabelle 5).
Schlussfolgerung
Die Kombination aus WBRT und SRS führte zu besserer IC und LC als die alleinige SRS, aber nicht zu besserem Gesamtüberleben. Da auch IC und LC wichtige Endpunkte sind, erscheint die zusätzliche WBRT bei Patienten mit 1 bis 3 Hirnmetastasen gerechtfertigt, insbesondere bei Patienten der RPA-Klasse I.
Similar content being viewed by others
References
Aoyama H, Shirato H, Tago M, et al. Stereotactic radiosurgery plus whole-brain radiation therapy vs stereotactic radiosurgery alone for treatment of brain metastases. A randomized controlled trial. JAMA 2006;295:2483–2491.
Brown PD, Asher AL, Farace E. Adjuvant whole brain radiotherapy: strong emotions decide but rationale studies are needed. Int J Radiat Oncol Biol Phys 2008;70:1305–1309.
Bruner DW, Wasserman T. The impact on quality of life by radiation late effects. Int J Radiat Oncol Biol Phys 1995;31:1353–1355.
Fahrig A, Ganslandt O, Lambrecht U, et al. Hypofractionated stereotactic radiotherapy for brain metastases-results from three different dose concepts. Strahlenther Onkol 2007;183:625–630.
Gaspar L E, Scott C, Rotman M, et al. Recursive partitioning analysis (RPA) of prognostic factors in three Radiation Therapy Oncology Group (RTOG) brain metastases trials. Int J Radiat Oncol Biol Phys 1997;37:745–751.
Joiner MC, Van der Kogel AJ. The linear-quadratic approach to fractionation and calculation of isoeffect relationships. In: Steel GG. Basic clinical radiobiology. New York: Oxford University Press; 1997:106–112.
Kaplan EL, Meier P. Non parametric estimation from incomplete observations. J Am Stat Assoc 1958;53:457–481.
Khuntia D, Brown P, Li J, et al. Whole-brain radiotherapy in the management of brain metastasis. J Clin Oncol 2006;24:1295–1304.
Meyers CA, Smith JA, Bezjak A, et al. Neurocognitive function and progression in patients with brain metastases treated with whole-brain radiation and motexafin gadolinium: results of a randomized phase III trial. J Clin Oncol 2004;22:157–165.
Nieder C, Astner ST, Grosu AL, et al. The role of postoperative radiotherapy after resection of a single brain metastasis. Combined analysis of 643 patients. Strahlenther Onkol 2007;183:576–580.
Piroth MD, Gagel B, Pinkawa M, et al. Postoperative radiotherapy of glioblastoma multiforme: analysis and critical assessment of different treatment strategies and predictive factors. Strahlenther Onkol 2007;183:695–702.
Pirzkall A, Debus J, Lohr F, et al. Radiosurgery alone or in combination with whole-brain radiotherapy for brain metastases. J Clin Oncol 1998;16:3563–3569.
O’Neill BP, Iturria NJ, Link MJ, et al. A comparison of surgical resection and stereotactic radiosurgery in the treatment of solitary brain metastases. Int J Radiat Oncol Biol Phys 2003;55:1169–1176.
Rades D, Bohlen G, Lohynska R, et al. Whole-brain radiotherapy with 20 Gy in 5 fractions for brain metastases in patients with cancer of unknown primary (CUP). Strahlenther Onkol 2007;183:631–636.
Regine WF, Huhn JL, Patchell RA, et al. Risk of symptomatic brain tumor recurrence and neurologic deficit after radiosurgery alone in patients with newly diagnosed brain metastases: results and implications. Int J Radiat Oncol Biol Phys 2002;52:333–338.
Regine WF, Scott C, Murray K, et al. Neurocognitive outcome in brain metastases patients treated with accelerated-fractionation vs. accelerated-hyperfractionated radiotherapy: an analysis from Radiation Therapy Oncology Group Study 91–04. Int J Radiat Oncol Biol Phys 2001;51:711–717.
Schoggl A, Kitz K, Reddy M, et al. Defining the role of stereotactic radiosurgery versus microsurgery in the treatment of single brain metastases. Acta Neurochir (Wien) 2000;142:621–626.
Sneed PK, Lamborn KR, Forstner JM, et al. Radiosurgery for brain metastases: is whole brain radiotherapy necessary? Int J Radiat Oncol Biol Phys 1999;43:549–558.
Sneed PK, Suh JH, Goetsch SJ, et al. A multi-institutional review of radiosurgery alone vs. radiosurgery with whole brain radiotherapy as the initial management of brain metastases. Int J Radiat Oncol Biol Phys 2002;53:519–526.
Trotti A, Byhardt R, Stetz J, et al. Common toxicity criteria: version 2.0. An improved reference for grading the acute effects of cancer treatment: impact on radiotherapy. Int J Radiat Oncol Biol Phys 2000;47:13–47.
Vogelbaum MA, Suh JH. Resectable brain metastases. J Clin Oncol 2006;24:1289–1294.
Yuan J, Wang JZ, Lo S, et al. Hypofractionation Regimens for Stereotactic Radiotherapy for Large Brain Tumors. Int J Radiat Oncol Biol Phys 2008;72:390–397.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rades, D., Kueter, JD., Hornung, D. et al. Comparison of stereotactic radiosurgery (SRS) alone and whole brain radiotherapy (WBRT) plus a stereotactic boost (WBRT + SRS) for one to three brain metastases. Strahlenther Onkol 184, 655–662 (2008). https://doi.org/10.1007/s00066-008-1946-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-008-1946-8